OBJECTIVE: To examine restrictions in daily functioning from a rehabilitation perspective in patients one year after discharge from the intensive care unit, and to identify prognostic factors for functional status.
DESIGN: Cross-sectional design.
Patients: Consecutive patients who were admitted to the intensive care unit for more than 48 h (n = 255).
METHODS: One year after intensive care, functional status (Sickness Impact Profile) as primary outcome, and Quality of Life (SF-36), anxiety and depression (Hospital Anxiety Depression Scale), and post-traumatic stress disorder (Impact of Events Scale) were evaluated.
RESULTS: Fifty-four percent of the patients had restrictions in daily functioning. Walking and social activities were most frequently restricted (30–60% of the patients). Quality of life was lower than the general Dutch population. Symptoms of anxiety and depression were found in 14%, and post-traumatic stress disorder in 18%. Severity of illness at admission and length of stay in the intensive care unit were identified as prognostic factors, although they explained only 10% of functional status.
CONCLUSION: The high prevalence of long-lasting restrictions in physical, social and psychological functioning among patients who stayed in the intensive care unit for at least 2 days implies that these patients are a potential target population for rehabilitation medicine. Multidisciplinary therapies need to be developed and evaluated in order to improve outcome.
Key words: critical illness, intensive care, rehabilitation, activities of daily living.
J Rehabil Med 2009; 41: 360–366
Correspondence address: Marike van der Schaaf, Department of Rehabilitation, Academic Medical Center, University of Amsterdam, PO Box 22660, NL-1100 DD Amsterdam, The Netherlands. E-mail: m.vanderschaaf@amc.uva.nl
Submitted July 14, 2008; accepted October 31, 2008
INTRODUCTION
Critical illness is associated with a wide range of serious long-lasting impairments that interfere with optimal functional outcome. Several studies have reported long-term physical impairments (1, 2), post-traumatic stress disorder (PTSD) (3), anxiety and depression (2) and reduced quality of life (QoL) (4) in survivors of the intensive care unit (ICU). To date, despite these problems within the different health domains, this patient group is not routinely referred to rehabilitation services.
The expertise of rehabilitation medicine could be beneficial to reduce the long-term restrictions in daily functioning, and to improve the long-term outcome of ICU survivors. In this respect, the relative contribution of restrictions in physical and psychosocial functioning on daily functioning may have considerable therapeutic consequences. Rehabilitation may focus on either physical or mental functioning, or both. For the planning of adequate rehabilitation care during convalescence after ICU discharge, a thorough understanding of the long-term functional restrictions from a rehabilitation perspective is a prerequisite.
Although the perceived QoL of ICU survivors has been studied extensively in the literature (4), little information is available on the impact of their health condition on daily functioning.
The aim of this cross-sectional study was to describe restrictions in daily functioning, and to identify prognostic factors for the functional status of critically ill patients one year after discharge from the ICU.
METHODS
Patients
This inception cohort study was undertaken in the Academic Medical Center of the University of Amsterdam, a 28-bed mixed closed-format adult ICU in a 1000-bed hospital. All patients admitted between June 2004 and June 2005 for more than 48 h in the ICU were considered eligible. The survival status and residential address of all ICU survivors were tracked by means of telephone calls with their general practitioner. Patients were considered to be lost to follow-up if their residential address could not be ascertained.
Measurements
Twelve months after discharge from the ICU, questionnaires were sent to all survivors. A follow-up letter was sent to all non-respondents, followed by a telephone call to obtain information about reasons for non-response.
The primary outcome was the Sickness Impact Profile 68 (SIP68) (5). The SIP68 is a validated short version of the 136-item version of the Sickness Impact Profile (SIP) and evaluates health-related functional status by assessing the behavioural impacts of sickness. The SIP68 consists of 6 domains (somatic autonomy, mobility control, psychic autonomy and communication, social behaviour, emotional stability and mobility range). A total SIP68 score and separate domain scores can be calculated, with scores ranging from 0 (no functional restrictions) to 100 (severe functional limitations). The cut-off point as recommended by Bosscha et al. (6) was applied, by which patients with a score of 0–10 were classified as doing well in daily life, scores in the range 11–20 indicated mild health-related dysfunctions, and scores > 20 indicated clear disablement in performing activities of daily living, i.e. poor functional status.
Secondary outcome measures were QoL (Medical Outcomes Study 36 Item Short form; SF-36) (7), symptoms of anxiety and depression (Hospital Anxiety and Depression Scale; HADS) (8, 9) and PTSD-related symptoms (Impact of Events Scale; IES) (10, 11). QoL was compared with normative data from the general Dutch population (7). For the presence of depression, anxiety or both, the cut-off level of 19, as recommended by Spinhoven et al. (12), was used. For the subscales anxiety and depression, the cut-off values of 11 or more according to Zigmond & Snaith (9) were applied. For the identification of severe coping disorders, scores above the cut-off point of 35 were classified as a high level of PTSD-related symptoms, in agreement with the previous findings of Neal et al. (13).
Dutch validated self-report versions of all outcome measures were used. Baseline data and information about potential risk factors for long-term functional status were obtained from medical records.
The Acute Physiology and Chronic Health Evaluation II (APACHE II) classification was used as one of the potential prognostic factors. The APACHE II classification measures the severity of disease for patients admitted to an ICU and is calculated from 12 routine physiological measurements (blood pressure, body temperature, heart rate, etc.) during the first 24 h after admission, information about previous health status and some information obtained at admission (such as age). Scores range from 0 to 71; higher scores imply a more severe disease and a higher risk of death (14).
Sociodemographics and information about other relevant outcome measures for functional status, such as employment status and living arrangements, were obtained by a questionnaire completed by the patients.
The study was submitted for approval to the local ethics committee, which waived the need for informed consent because of the non-interventional nature of the study.
Statistical analysis
The baseline data and outcome measures were analysed with descriptive statistics. The data are expressed as mean and standard deviation (SD) and, in case of a skewed distribution, medians and interquartile ranges are presented. The mean SF-36 scale scores of ICU patients at baseline were compared with those of the age-matched Dutch general population using the Z-score (difference between patient and Dutch general population mean score, divided by general population SD), whereas a value of ≥ 0.8 represents a difference of at least four-fifths the SD and is viewed as a deviation from the norm score (15).
Univariate and multivariate logistic regression analyses, with SIP68 as dependent variable (cut-off point > 20, i.e. poor functional status), were performed to determine the predictive ability of the potential prognostic variables, gender, age, severity of illness on ICU admission (APACHE II) (14), length of stay (LOS) in ICU, and admission diagnosis category. First, all variables were entered as independent variables in the univariate analyses. In addition, all independent variables were then entered in order of p-value obtained in the univariate regression analyses into a multivariate logistic regression model (forward selection procedure). The relationship between poor functional status and symptoms of anxiety and depression, and PTSD were investigated with the Spearmans’s rho correlation coefficient. A p-value of < 0.05 was considered to be statistically significant. All statistical analyses were performed in SPSS 12.0 (SPSS Inc, 444 North Michigan Ave, Chicago, IL 60611, USA).
RESULTS
Of the 1738 patients who were admitted to the ICU, there were 746 eligible patients who stayed more than 48 h in the ICU. The ICU mortality rate was 13%, and the overall hospital mortality rate was 26%. Of all 555 ICU survivors who had been discharged from the hospital the survival status and residential address were tracked. Twelve months after discharge an additional 87 (16%) patients had died and 42 (8%) patients could not be traced.
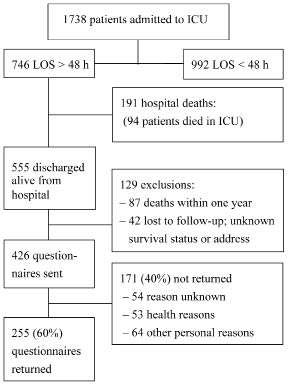
Patients who survived but could not be traced (n = 42) were younger than the other survivors (n = 426, p = 0.02), but there was no significance difference in gender, LOS in the ICU, or APACHE II score on admittance. Questionnaires were sent to all 426 survivors with a known address, 255 (60%) of whom completed and returned the questionnaires. Reasons for not returning the questionnaire were “ill-health” (45%), and “other, non-medical, personal reasons” (55%). The number of survivors, the excluded patients, and patients included in the data analysis are presented in the flow diagram in Fig. 1.
Fig. 1. Flow diagram of study participants. ICU: intensive care unit, LOS: length of stay.
Table I presents the characteristics of all ICU patients and of the “respondents” and “non-respondents”. There were no differences in age, LOS in the ICU, duration of ventilation and the APACHE II score between the respondents and the non-respondents within the entire group of ICU survivors.
Respondents admission diagnostic categories in ICU included medical reasons in 33% of the patients (mostly respiratory failure), non-scheduled surgery in 24% (21 abdominal and trauma, 23 neurosurgery, 12 cardiothoracic, 6 other), and scheduled surgery in 43%, (83 cardiothoracic, 21 abdominal, 7 other).
Primary outcome SIP68
One year after discharge, the total median SIP68 score was 11 (interquartile range 3–26). Table II summarizes the SIP68 scores of 253 patients. Forty-six percent of the patients had a score with which they were expected to be doing well in daily life (score 0–10), 22% had mild dysfunctions (score 11–20) and 32% had poor functional status (score > 20).
| Table I. Demographic data of the study population |
| | All ICU patients LOS > 48 h (n = 746) | Patients alive after one year (n = 426) |
| Non-respondents (n = 171) | Respondents (n = 255) | p-value* |
| Age, years, mean (SD) [range] | 59.9 (16.6) [18–91.7] | 58.9 (16.3) [18.6 –90.4] | 58.8 (16.6) [18–84.7] | 0.98 |
| Gender, male/female, n (%) | 485 (65)/261 (35) | 97 (57)/74 (43) | 169 (66)/86 (34) | 0.06 |
| ICU stay, days Mean (SD) [min–max] Median (25th-75th percentile) | 9.6 (13) [2–169] 5.4 (3.1–10) | 8.2 (9) [2–58] 4.9 (3.2–8.9) | 8.7 (10) [2–62] 5 (3.0–9.3) | 0.53 |
| Mechanical ventilation, days Mean (SD) [min–max] Median (25th-75th percentile) | 7.3 (11) [0–169] 4 (2–8) | 5.5 (6) [0–38] 4 (2–7) | 6.5 (8) [0–49] 4 (2–7) | 0.15 |
| APACHE II Mean (SD) [min–max] | 15.7 (6) [2–35] | 14.7 (5.4) [3– 28] | 14.5 (6) [2–35] | 0.76 |
| Admission diagnosis, n (%) Medical† Unscheduled surgery Scheduled surgery | 343 (46) 172 (23) 231 (31) | 84 (49) 35 (20) 52 (30) | 83 (33) 62 (24) 110 (43) | 0.002 |
| *The independent sample t-test was used for continuous variables, and the χ2 test was used for the categorical variables. †Medical: no surgery in past 7 days prior to ICU admission. ICU: intensive care unit; LOS: length of stay; APACHE: Acute Physiology and Chronic Health Evaluation score; SD: standard deviation. |
| Table II. Functional status according to the Sickness Impact Profile 68 (SIP68) (n = 253). Score range 0–100 |
| SIP68 | Median | P25– P75 | Range |
| Somatic autonomy | 0 | 0–6 | 0–88 |
| Mobility control | 8 | 0–33 | 0–100 |
| Psychic autonomy and communication | 0 | 0–27 | 0–100 |
| Social behaviour | 25 | 8–50 | 0–100 |
| Emotional stability | 0 | 0–17 | 0–100 |
| Mobility range | 0 | 0–20 | 0–100 |
| Total SIP68 score | 11 | 3–26 | 0–77 |
| P25–P75: interquartile range. |
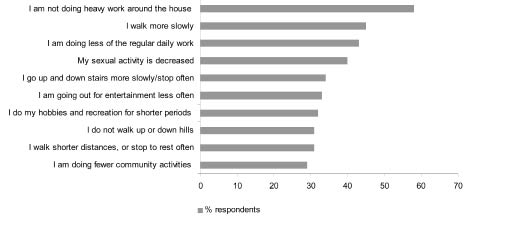
The highest percentage of dysfunctional items was found in the categories of social behaviour and mobility control. The social behaviour category describes the possible consequences of a health disorder on a person’s functioning in relation to other persons. Within this category more than 25% of the respondents reported that visiting friends, recreational and social activities, and sexual activity were restricted, compared with prior ICU functioning. The mobility control category describes behaviour that is related to the level of control that an individual has over his or her own body (5). In this category, more than 25% of the respondents reported being restricted in activities related to walking, such as walking slowly and problems with walking stairs, hills, and distances. The top 10 of most commonly reported problems (SIP68) are presented in Fig. 2.
Compared with physical and social activities, activities related to psychological functioning were less reported to be restricted. However, in the category psychic autonomy and communication, 25–27% reported difficulty with respect to reasoning and solving problems, impaired concentration and short-term memory. Within the category emotional stability, 20% mentioned acting irritably, being impatient, and not joking with family members as they used to do.
Quality of life, symptoms of anxiety and depression and PTSD
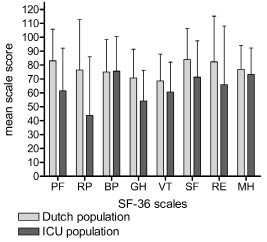
The SF-36 scores are summarized in Table III. The values of the Z-scores of the SF-36 scales Physical Function, Role Physical, and General Health were lower than the general Dutch population (≤ –0.8). Fig. 3 shows the SF-36 mean scale scores for the study sample and the normative data of a general Dutch population sample.
| Table III. Quality of life and psychosocial functioning in intensive care unit (ICU) survivors after 12 months |
| Measurements | Median | P25– P75 | Range | Mean (SD) | Mean Z score |
| SF-36 (n = 250) | | | | | |
| Physical function (0–100) | 65 | 35–90 | 0–100 | 61 (31) | –0.95* |
| Role physical (0–100) | 25 | 0–100 | 0–100 | 44 (42) | –0.90* |
| Bodily pain (0–100) | 80 | 55–100 | 0–100 | 76 (25) | 0.03 |
| General health (0–100) | 55 | 40–75 | 0–100 | 54 (22) | –0.81* |
| Vitality (0–100) | 65 | 45–75 | 0–100 | 61 (22) | –0.42 |
| Social function (0–100) | 75 | 56–100 | 0–100 | 71 (26) | –0.57 |
| Role emotional (0–100) | 100 | 33–100 | 0–100 | 66 (42) | –0.50 |
| Mental health (0–100) | 76 | 66–88 | 0–100 | 73 (19) | –0.20 |
| HADS (n = 247) | | | | | Cut-off, n (%) |
| HADS anxiety (0–21) | 4 | 1–7 | 0–20 | | > 10, n = 28 (11%) |
| HADS depression (0–21) | 3 | 1–7 | 0–20 | | > 10, n = 28 (11%) |
| HADS Total score (0–42) | 7 | 2–14 | 0–38 | | > 19, n = 34 (14%) |
| IES (n = 238) | | | | | |
| IES intrusion (0–35) | 4 | 0–15 | 0–35 | | |
| IES avoidance (0–40) | 5 | 0–13 | 0–40 | | |
| IES Total score (0–75) | 10 | 1–29 | 0–75 | | > 35, n = 43(18%) |
| *A value of –0.8 or smaller indicates a deviation from the norm score. Prevalence, anxiety and depression, post traumatic stress disorder related symptoms according to the clinical cut-off points. n (%) = number (%) of patients with scores above the clinical cut-off point. SF-36 negative Z-scores indicating impaired functioning compared with the general population (mean and standard deviation (SD)). SF-36: medical outcomes study 36-item Short-Form health survey; higher scores representing better functioning; HADS: Hospital Anxiety and Depression Scale; higher scores representing poor functioning; IES: Impact of Events Scale; higher scores representing poor functioning; P25–P75: interquartile range. |
Fig. 3. 36-item Short-Form health survey (SF-36) mean scale scores for the study sample and the Dutch general population sample. PF: physical function; RP: role physical; BP: bodily pain; GH: general health; VT: vitality; SF: social function; RE: role emotional; MH: mental health; ICU: intensive care unit.
The median score on the HADS was 7 (interquartile range 2–14), and 34 (14%) of the patients were found to have symptoms of anxiety and depression (Table III). The HADS score was associated with poor functional status (SIP > 20; Spearman’s rho HADS r = 0.478, p < 0.000). Of the patients with anxiety and depression (HADS > 19), 74% also had poor functional status (SIP > 20).
The median score on the IES was 10 (interquartile range 1–29) (Table III), and 43 (18%) respondents were found to have symptoms of PTSD. The IES score was associated with functional status (Spearmans’s rho IES
and SIP68 r = 0.260, p < 0.000). However, within the group of patients with symptoms of PTSD (IES > 35), 50% had poor functional status, and 50% did not.
Changes in living arrangements and employment status
One year after discharge from the ICU the living arrangements of only 7 patients had changed; of the 240 patients previously living independently, 4 had moved to a nursing home and 3 had temporarily moved in with their parents.
Of the 82 patients who were employed before ICU admission, only 54% (44) had resumed their previous employment after one year. The percentage of patients on sick leave increased from 2% (5) prior to ICU admission to 15% (37) (Table IV).
| Table IV. Source of income of intensive care unit (ICU) survivors (n = 251) |
| | Pre-ICU admission | One year after discharge |
| Job | 82 (33%) | 44 (18%) |
| Retirement | 107 (43%) | 113 (45%) |
| Invalidity pension | 34 (14%) | 33 (13%) |
| Temporary sick leave | 5 (2%) | 37 (15%) |
| Other source* | 23 (9%) | 24 (10%) |
| *Partners income, welfare, student scholarship. |
Referral for rehabilitation
After discharge from the ICU, 22 (9%) patients were transferred to a rehabilitation facility and another 50 (20%) followed an outpatient multidisciplinary rehabilitation programme. Patients referred for rehabilitation were younger (p = 0.03), but did not differ from the patients who were not referred, with respect to LOS (p = 0.1), APACHE (p = 0.2) or admission diagnosis p = 0.06). Of these 72 patients, 40 (67%) still participated in a multidisciplinary rehabilitation programme after one year.
Of all ICU survivors, 32 (13%) still received medical attention from a rehabilitation physician, 92 (37%) received physical therapy, 34 (14%) were treated by a psychologist, and 31 (12%) by a social worker, 9–12 months after discharge. Patients who participated in a multidisciplinary rehabilitation programme after one year had worse functional status compared with those who did not (SIP68 p = 0.006). Of the patients with a residual poor functional status, 20% (16) reported that they received medical attention from a rehabilitation physician in the preceding 3 months, 7 of whom received multidisciplinary interventions (treatment by a rehabilitation physician, and 2 or more other disciplines, such as physical therapy, occupational therapy, psychiatrist, psychologist or social worker). Half of the patients with poor functional status had physical therapy. Of the patients with psychological distress (HADS > 19, or IES > 35), 24% received treatment from a psychiatrist, psychologist or social worker.
Potential prognostic factors for functional status
Univariate analysis showed that the APACHE score on ICU admission, the LOS in the ICU and the admission diagnosis category were significantly associated with poor functional status (APACHE p = 0.017, r = 0.15, LOS p = 0.012, r = 0.158, admission diagnosis p = 0.019, r = 0.147). Acute admitted patients (acute surgery and medical) had a poorer functional status than elective patients (elective surgery). The final model of the logistic multivariate regression analyses model with poor functional status (SIP68 > 20) as the dependent variable included ICU LOS and APACHE II (odds ratio 1.047, 95% confidence interval 1.002–1.095, p = 0.043). The percentage of the variance explained by the model was 9.8%.
DISCUSSION
This study shows that one year after discharge from the ICU, patients who were treated for at least 2 days in the ICU, had great limitations in physically related activities, in particular walking activities, and many problems in social functioning. It was also found that disease-related factors early after ICU discharge are not of sufficient clinical value to identify patients who are at risk of poor functional status.
One year after discharge from the ICU, more than half of the survivors of a critical illness had restrictions in daily functioning, resulting in reduced physical, social and psychological well-being. One-third of all participants had poor functional status (SIP68 > 20). With this, activities within the SIP68 categories mobility range and social behaviour, which, with the exception of sexual activity, all require good walking capacity and physical endurance, were most commonly reported to be restricted. To illustrate, 30–60% reported walking more slowly, walking shorter distances, having difficulties with stairs and hills, going out for entertainment less often, spending less time on hobbies, recreation and community activities (Fig. 2). With respect to the high percentage of patients reporting decreased sexual activity (40%; Fig. 2), we found that these patients had significantly higher scores on all SIP68 domains (indicating poorer functioning), which indicates that this may be associated with problems in both physical and psychological functioning. Activities related to the psychic autonomy and communication category were less reported to be restricted. However, an incidence of 25% of the patients reporting difficulty reasoning and solving problems, and impaired concentration and short-term memory is still very high. These findings are in accordance with the findings of Hopkins & Jackson (16), who also reported impairments in executive function, mental processing speed, attention and memory in ICU survivors. Thereby, one should take into account that neurocognitive impairments appear to be under-recognized in ICU patients (16). With this, we believe that limitations in walking capacity and physical endurance, concentration and memory problems, have a great impact on daily functioning in ICU survivors. To illustrate, the return to work rate in this study was 46%, which is in agreement with previous studies in ICU survivors, and shows that the impairments in functioning may have important consequences for participation and may lead to substantial economic costs (1, 17).
Fig. 2. Top 10 frequency item scores on the Sickness Impact Profile 68.
The second important finding is that the identification of patients who are most likely to develop long-term problems in functional status is not possible shortly after discharge from the ICU, on the basis of information regarding gender, age, admission diagnosis, severity of illness on admission, and LOS in the ICU. Although significant associations between QoL and these factors have been identified in several studies, as reported in a systematic review by Dowdy et al. (4), its clinical value with respect to the identification of patients who are at risk of poor functional status has not been studied previously. In the present study, only 9.8% of the variance of poor functional status was explained by ICU LOS and APACHE II score.
In this study population, perceived QoL after one year is in accordance with other studies that used the SF-36 as reported in a meta-analysis (18). Compared with previous studies, in which the functional status of patients from the ICU was assessed with the SIP (19–21), the 32% prevalence of severe disability found in this study is rather high. The relatively poor outcome in the present study, compared with that reported in the literature, may be due to the selection criteria that we applied. We evaluated patients with an ICU stay > 48 h, whereas other studies using the SIP in ICU populations have also included patients with a shorter LOS in the ICU.
The incidences of symptoms of anxiety, depression and PTSD in our study are in agreement with the range of incidences found in previous studies (2, 3, 22, 23). The interpretation of the scores (SIP68, HADS, IES) depends on the choice of cut-off points. In the present study high cut-off points were used, which may have resulted in an under-estimation of the actual prevalence of restrictions in functional status, anxiety and depression, and PTSD.
With respect to the association between functional restrictions and symptoms of psychological distress, we conclude that, especially in patients with poor functional status, attention should be focused not only on physical restrictions, but also on symptoms of anxiety and depression. By contrast, symptoms of PTSD were found in patients regardless of their functional health status and should therefore be monitored in all patients.
Our study could be criticized for failing to document the health status of patients prior to ICU admission. Ideally, one would want to distinguish whether the observed functional reflects functioning prior to ICU admission or the long-term effect of critical illness. In our ICU, the vast majority of the patients are acute admissions by which pre-admission data-acquisition is not possible. Information on functional health prior to ICU admission can, to a certain extent, also be inferred from surrogate measures, such as living arrangements and source of income. Prior to ICU admission the majority of the patients were living independently, 14% received an invalidity pension and only 2% were on temporary sick leave. In addition, the SIP68 measures change in daily functioning due to sickness. Therefore, we believe that the restrictions that we found one year after discharge from the ICU, could primarily be considered as long-term consequences of the critical illness.
Another limitation of this study is the possibility of selection bias. This study had a 60% response rate, which is in accordance with other follow-up studies in ICU populations (3, 21, 24). With regard to the reasons for not returning the questionnaire, the reason given by 45% of the non-respondents was poor health, and 55% mentioned personal reasons that were not related to health status. Additional analysis suggests that, except for gender, the baseline demographic characteristics, APACHE II score on admission, and LOS in the ICU were similar between respondents and non-respondents (Table I). Therefore, it seems likely that the SIP68 scores of the respondents are also representative of the non-respondents, although selection bias cannot be ruled out.
In this cross-sectional study we are unable to provide information on the course of recovery during the first year, or the extent to which the present restrictions can further be reduced. Studies evaluating QoL have shown that recovery is incomplete after one year, and that convalescence may take up to 14 years (4). Therefore, some recovery potential in the performance of daily activities can be anticipated in the majority of the patients with restricted functioning. In our study population, only a minority of patients with a poor functional status or with high levels of psychological distress received attention from rehabilitation services. The literature on the referral to rehabilitation therapy of patients from ICU is scarce; however, in a study by Hopkins et al. (17), it was found that impairments in mental functions are frequently overlooked in patients from ICU. We believe that in patients with poor functional status, and in patients with high levels of psychological distress who did not receive rehabilitation treatment, recovery might have been improved if specifically targeted rehabilitation treatment had been provided. However, to date, little evidence has been available with respect to the effectiveness of rehabilitation interventions on patients after a critical illness (25, 26).
The findings of this study have significant clinical implications for the planning of care after ICU discharge. Whereas survival and QoL in previous studies have been regarded as relevant outcomes after a stay in the ICU (19–21), the observations of functional restrictions in the present study should be considered as important directions to target interventions aimed at improving the outcomes of ICU patients. In our opinion, patients who survive a critical illness deserve attention from the field of rehabilitation medicine. Exercise programmes aiming at improvement in walking capacity and endurance may be beneficial for patients who are discharged from the ICU. Furthermore, in the rehabilitation treatment of critically ill patients one should take into account the high prevalence of psychological distress and concentration and memory problems. Since known prognostic factors had only limited predictive value for the development of functional restrictions, a longitudinal follow-up of patients with an ICU length of stay of at least 2 days might clarify further which patients are at risk of functional limitations.
Future research should examine the contribution of potential prognostic factors in functional recovery, and the effect of interventions aiming at the improvement of functional outcome in patients after discharge from the ICU.
ACKNOWLEDGEMENT
We wish to thank Marijke Rijpstra for her assistance with data collection.
REFERENCE
1. Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, az-Granados N, Al-Saidi F, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med 2003; 348: 683–693.
2. Sukantarat K, Greer S, Brett S, Williamson R. Physical and psychological sequelae of critical illness. Br J Health Psychol 2007; 12: 65–74.
3. Jackson JC, Hart RP, Gordon SM, Hopkins RO, Girard TD, Ely EW. Post-traumatic stress disorder and post-traumatic stress symptoms following critical illness in medical intensive care unit patients: assessing the magnitude of the problem. Crit Care 2007; 11: R27.
4. Dowdy DW, Eid MP, Sedrakyan A, Mendez-Tellez PA, Pronovost PJ, Herridge MS, et al. Quality of life in adult survivors of critical illness: a systematic review of the literature. Intensive Care Med 2005; 31: 611–620.
5. de Bruin AF, Diederiks JP, de Witte LP, Stevens FC, Philipsen H. The development of a short generic version of the Sickness Impact Profile. J Clin Epidemiol 1994; 47: 407–418.
6. Bosscha K, Reijnders K, Jacobs MH, Post MW, Algra A, van der Werken C. Quality of life after severe bacterial peritonitis and infected necrotizing pancreatitis treated with open management of the abdomen and planned re-operations. Crit Care Med 2001; 29: 1640–1641.
7. Aaronson NK, Muller M, Cohen PD, Essink-Bot ML, Fekkes M, Sanderman R, et al. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol 1998; 51: 1055–1068.
8. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002; 52: 69–77.
9. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67: 361–370.
10. Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med 1979; 41: 209–218.
11. van der Ploeg, Mooren TT, Kleber RJ, van der Velden PG, Brom D. Construct validation of the Dutch version of the impact of event scale. Psychol Assess 2004; 16: 16–26.
12. Spinhoven P, Ormel J, Sloekers PP, Kempen GI, Speckens AE, Van Hemert AM. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med 1997; 27: 363–370.
13. Neal LA, Busuttil W, Rollins J, Herepath R, Strike P, Turnbull G. Convergent validity of measures of post-traumatic stress disorder in a mixed military and civilian population. J Trauma Stress 1994; 7: 447–455.
14. Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE. APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med 1981; 9: 591–597.
15. Cohen J, editor. Statistical power analysis for the behavioural sciences. 1977 edn. New Jersey: Lawrence Erlbaum Associates, Inc.; 1977.
16. Hopkins RO, Jackson JC. Long-term neurocognitive function after critical illness. Chest 2006; 130: 869–878.
17. Hopkins RO, Weaver LK, Collingridge D, Parkinson RB, Chan KJ, Orme JF Jr. Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome. Am J Respir Crit Care Med 2005; 171: 340–347.
18. Dowdy DW, Eid MP, Dennison CR, Mendez-Tellez PA, Herridge MS, Guallar E, et al. Quality of life after acute respiratory distress syndrome: a meta-analysis. Intensive Care Med 2006; 32: 1115–1124.
19. Gardner A, Sibthorpe B. Will he get back to normal? Survival and functional status after intensive care therapy. Intensive Crit Care Nurs 2002; 18: 138–145.
20. Short TG, Buckley TA, Rowbottom MY, Wong E, Oh TE. Long-term outcome and functional health status following intensive care in Hong Kong. Crit Care Med 1999; 27: 51–57.
21. Tian ZM, Miranda DR. Quality of life after intensive care with the sickness impact profile. Intensive Care Med 1995; 21: 422–428.
22. Girard TD, Shintani AK, Jackson JC, Gordon SM, Pun BT, Henderson MS, et al. Risk factors for post-traumatic stress disorder symptoms following critical illness requiring mechanical ventilation: a prospective cohort study. Crit Care 2007; 11: R28.
23. Jones C, Backman C, Capuzzo M, Flaatten H, Rylander C, Griffiths RD. Precipitants of post-traumatic stress disorder following intensive care: a hypothesis generating study of diversity in care. Intensive Care Med 2007; 33: 978–985.
24. Granja C, Lopes A, Moreira S, Dias C, Costa-Pereira A, Carneiro A. Patients’ recollections of experiences in the intensive care unit may affect their quality of life. Crit Care 2005; 9: R96–R109.
25. Jones C, Skirrow P, Griffiths RD, Humphris GH, Ingleby S, Eddleston J, et al. Rehabilitation after critical illness: a randomized, controlled trial. Crit Care Med 2003; 31: 2456–2461.
26. Jones C, Capuzzo M, Flaatten H. ICU diaries may reduce symptoms of posttraumatic stress disorder. Intensive Care Med 2006; 32 Suppl 1: S144.