OBJECTIVE: To develop a questionnaire (ABILOCO-Kids) based on the Rasch measurement model that assesses locomotion ability in children with cerebral palsy.
DESIGN: Prospective study and questionnaire development.
SUBJECTS: A total of 113 children with cerebral palsy (10 (standard deviation 2.5) years old).
METHODS: A 41-item questionnaire was developed based on existing scales and on the clinical experience of professionals in the field of rehabilitation. This questionnaire was tested separately on the 113 children with cerebral palsy and their parents. Their responses were analysed using the Rasch model (RUMM-2020®) to select items that had an ordered rating scale and that fit a unidimensional model.
RESULTS: The final ABILOCO-Kids scale consisted of 10 locomotion activities, of which difficulty was rated by the parents. The parents gave a more precise assessment of their children’s ability than the children themselves, leading to a wider range of measurement that was well-targeted on the sample population and that had good reliability (r = 0.97) and reproducibility (intraclass correlation coefficient = 0.96). Item calibration did not vary with age, sex or clinical presentation (hemiplegia, diplegia, quadriplegia). The concurrent validity of the ABILOCO-Kids questionnaire was also shown by its correlation with the Gross Motor Function Classification System.
CONCLUSION: The ABILOCO-Kids questionnaire has good psychometric qualities for measuring a wide range of locomotion abilities in children with cerebral palsy.
Key words: locomotion, questionnaire, children, cerebral palsy, outcome assessment.
J Rehabil Med 2008; 40: 823–830
Correspondence address: Gilles D. Caty, Université catholique de Louvain, Cliniques universitaires Saint-Luc, Physical Medicine and Rehabilitation Department, Avenue Hippocrate 10, BE-1200 Brussels, Belgium. E-mail: Gilles.Caty@uclouvain.be
Submitted October 30, 2007; accepted June 12, 2008
INTRODUCTION
Cerebral palsy (CP) is the leading cause of physical disability among children (1). The neurological impairments in children with CP frequently limit walking ability, which is an activity essential for daily life activities and social participation (International Classification of Functioning, Disability and Health (ICF) model World Health Organisation (WHO) (2)). New therapeutic approaches are continuously being developed for the management of locomotor impairment in individuals with CP (3). Some of these new strategies are intended to reduce spasticity (4) (e.g. intramuscular botulinum toxin, intrathecal baclofen administration or dorsal rhizotomy), while others aim to improve locomotion ability using sophisticated orthoses (5) or multilevel surgery (6). The efficacy of these treatments on locomotion activity should be appraised using appropriate clinical assessment tools. In addition, the ability of children to walk may change during growth (7) and needs to be assessed over time (8).
Several scales are available to assess locomotion ability in the activity domain of the ICF (2) among children with CP: the Gross Motor Function Measure (9) (GMFM) and the Gross Motor Function Classification System (10) (GMFCS), the Pediatric Evaluation of Disability Inventory (11) (PEDI), the Activities Scale for Kids (12) (ASK), the Functional Independence Measure for Children (13) (WeeFIM), the Functional Mobility Scale (14) (FMS) and the Gillette Functional Assessment Questionnaire (15) (FAQ). These validated and reliable scales are widely used in the assessment of children with CP (Table I). Unfortunately, these tools present some limitations in the measurement of walking ability. Indeed, they are not specific for walking ability; the GMFM, the PEDI and the ASK measure the physical disability as a whole and the WeeFIM measures a child’s functional performance in daily life activities (e.g. self-care, social function, and mobility). These 4 scales require 15–45 min to be administered by skilled staff. On the contrary, the FMS and the FAQ are focused on walking ability and are easily and quickly administered. The psychometric properties (unidimensionality and linearity) of the GMFM-66, the PEDI, the ASK and the WeeFIM have been proven by Rasch analysis (16–17). The latent variable measured by these scales is the global physical ability. The WeeFIM is invariant across age and the GMFM-66 is invariant across age and disability. The FAQ and the FMS have not been submitted to Rasch analysis. These 2 tools are ordinal scales that permit only limited computation and low power, non-parametric statistical analysis (18–19).
| Table I. Different scales to assess locomotion ability in children with cerebral palsy |
| | Rasch analysis |
| Scale | Psychometrics properties | Structure and domains | Time of administration (min) | Linearity Interval scale | Latent variable unidimensionality | Invariance DIF test |
| PEDI | Reliability ⊕ Validity ⊕ Inter-examiner reproducibility ⊕ | 237 items 3 domains | 45 | Yes | Physical disability | No |
| ASK | Reliability ⊕ Validity ⊕ Responsiveness ⊕ | 30 items 9 domains | 30 | Yes | Physical disability | No |
| WeeFIM | Reliability ⊕ Validity ⊕ Inter-examiner reproducibility ⊕ | 18 items 6 domains | 15 | Yes not specific for CP | Functional performance | Yes (age) |
| GMFM-66 | Reliability ⊕ Validity ⊕ Responsiveness ⊕ | 66 items 5 domains | 45 | Yes | Gross motor ability | Yes (ability) |
| GMFCS | Reliability ⊕ Validity ⊕ Inter-examiner reproducibility ⊕ | A 5-level ordinal grading classification focusing on mobility | A few | No | | |
| FAQ | Validity ⊕ Inter-examiner reproducibility ⊕ | A 10-level ordinal scale focusing on functional mobility | A few | No | | |
| FMS | Reliability ⊕ Validity ⊕ | A 6-level ordinal scale focusing on functional mobility | A few | No | | |
| ⊕ indicate that the scale presents this psychometric property. PEDI: Pediatric Evaluation of Disability Inventory; ASK: Activities Scale for Kids; WeeFIM: Functional Independence Measure for Children; GMFM: Gross Motor Function Measure; GMFCS: Gross Motor Function Classification System; FAQ: Gillette Functional Assessment Questionnaire; FMS: Functional Mobility Scale; DIF: Differential Item Functioning. |
In addition to these scales, there are gait laboratories that can perform extensive locomotion analyses that are especially useful for treatment planning. For instance, the results of these analyses can be used to select overactive muscles for chemodenervation or to choose an appropriate surgical approach (20). However, the artificial and highly motivating clinical environment of the gait laboratory may poorly reflect a child’s walking ability during daily life activities. The effect of treatment should not be limited to gait analysis but should also include an assessment of walking ability in the community.
The purpose of this study was to develop a questionnaire (ABILOCO-Kids) assessing the walking ability of children with CP focusing on the activity domain of the ICF. A Rasch analysis (16, 17) was applied to select items respecting the principles of linearity, unidimensionality and invariance.
Locomotion ability (ABILOCO) can be inferred from a patient’s or proxy reporter’s perception of the difficulty of performing locomotion activities. The use of parents as proxy reporters is advised for very young children and for teenagers (21). The preliminary questionnaire was, therefore, given to children and to their parents in order to compare the reliability of the reported perceptions.
METHODS
Participants
The definition adopted for CP was “all non-progressive but often changing motor impairment syndromes secondary to lesions or anomalies of the brain arising in the early stages of its development” (22). A total of 113 children were recruited from 7 centres involved in the care of children with CP (Table II). Because ABILOCO-Kids was designed as an interview-based questionnaire, children with a major intellectual deficit (IQ < 60) or who were younger than 6 years of age were excluded. Unfortunately, 5 parents did not complete the questionnaire. The final sample was thus made up of 113 children and 108 parents.
| Table II. Subject characteristics (n = 113) |
| Characteristics | |
| Age, years, mean (SD) [range] | 10 (2.5) [6–15] |
| Sex | |
| Male | 67 |
| Female | 46 |
| Type of cerebral palsy | |
| Quadriplegia/paresis | 35 |
| Diplegia | 24 |
| Hemiplegia/paresis | |
| Right | 26 |
| Left | 28 |
| GMFCS | |
| Level I: most independent motor function | 50 |
| Level II | 26 |
| Level III | 12 |
| Level IV | 21 |
| Level V: least independent motor function | 4 |
| GMFCS: Gross Motor Function Classification System; SD: standard deviation. |
The study was approved by the ethics committee of our Medical School.
Questionnaire development
The preliminary questionnaire included a large sample of activities corresponding to the ICF definition of locomotion (2): the individual’s ability to move about effectively in their environment, as classified in the Activity domain. Item selection was also based on a review of existing scales (GMFM, PEDI, ASK, WeeFIM and FAQ) and on the experience of our rehabilitation team. The first version of ABILOCO-Kids included a pool of 41 items (Table III).
| Table III. The 41-item preliminary questionnaire |
| 1. | Running on all types of surfaces. |
| 2. | Walking between parallel bars. |
| 3. | Walking alone outside on all types of surfaces. |
| 4. | Taking the train or the underground railway. |
| 5. | Walking while holding a fragile object (such as a full glass). |
| 6. | Kicking a ball with the paretic foot. |
| 7. | Walking several minutes at the same speed as a healthy child. |
| 8. | Going up stairs putting both feet on each step. |
| 9. | Stepping up a kerb alone. |
| 10. | Running correctly even if you have to turn. |
| 11. | Walking few steps with the help of a person. |
| 12. | Walking more than 5 metres with a rollator. |
| 13. | Walking with the help of a person who guides but doesn’t support. |
| 14. | Walking more than 5 metres with a crutch. |
| 15. | Walking more than 5 metres alone, indoors, on flat ground without an assistive device. |
| 16. | Jumping the height of 1 step of stairs. |
| 17. | Hopping on the healthy foot. |
| 18. | Going down stairs putting both feet on each step. |
| 19. | Turning and walking in a narrow place. |
| 20. | Walking less than 5 metres, indoors, holding onto pieces of furniture. |
| 21. | Ice-skating, skate boarding, roller-skating. |
| 22. | Taking the bus alone. |
| 23. | Running on regular and flat ground. |
| 24. | Walking less than 5 metres alone without the help of a person. |
| 25. | Going up and down stairs without holding onto the banisters. |
| 26. | Running with a tricycle. |
| 27. | Kicking a ball with the healthy foot. |
| 28. | Skipping rope. |
| 29. | Going down stairs putting each foot on the next step. |
| 30. | Hopping on the affected foot. |
| 31. | Striding over an object with the paretic foot first. |
| 32. | Walking more than 5 metres, alone, outside on flat ground. |
| 33. | Walking with the help of 2 persons who support. |
| 34. | Striding over an object with the healthy foot first. |
| 35. | Riding a bike. |
| 36. | Going up an escalator alone. |
| 37. | Going up and down stairs with the help of a handrail. |
| 38. | Walking backwards. |
| 39. | Going up stairs putting each foot on the next step. |
| 40. | Riding a bike with a stabilizer. |
| 41. | Walking while holding an object. |
Procedures
The 41-item questionnaire was administered separately to the children and to their parents in order to compare the reliability of the reported perceptions. The activities were presented in a random order to avoid any systematic effect. Ten different random orders of presentation were used. Each item was presented verbally to the child by the examiner, while the parents completed the questionnaire by themselves in another room. For each question, the children and their parents were asked to estimate, using a 3-level rating scale (0 = impossible, 1 = difficult, and 2 = easy), their perceived difficulty in performing that locomotion activity. Activities not attempted in the last 3 months or those for which they could not estimate the difficulty, were not scored and were encoded as missing responses. However, when an activity was never attempted because it was impossible, it was scored as “impossible”.
Data analysis
The responses from the children and those from their parents were analysed separately (RUMM2020 software, RUMM Laboratory Pty Ltd, Perth, Western Australia). The Rasch model (16) allows the total raw scores to be converted into linear measures. This model requires that only the item difficulty, the patient’s ability and the threshold difficulties determine the probabilities of endorsing any given category. Measurement units are expressed in logits (log-odds units), a probability unit that expresses the natural logarithm of the odds of success (i.e. the pass to fail probability ratio). At any given ability level, 1 logit difference between 2 patients indicates that their odds of successful achievement of any activity are 2.7:1 (i.e. e1:1). The logit metric provides a linear unit, representing a fixed increment along the whole scale of the explored variable. Analyses were performed with the rating scale and partial credit models (23).
Item selection
Successive analyses were used to select the items that constituted the final ABILOCO-Kids scale. Items that did not meet any of the following criteria were eliminated.
The first selection criterion was the frequency of missing values. Only items with a response rate higher than 90%, indicating that the children in our sample commonly attempted them and that these activities are relevant to measure their locomotion ability, were retained.
The second criterion was the order of thresholds between successive response categories (ordered scale). The thresholds of each item correspond to the locomotion ability levels required to have an equal probability of endorsing one response rather than the previous one. If the anticipated order of response categories was verified, subjects with greater locomotion ability should have selected a higher response for any given item and subjects selecting a higher response for a given item should have had greater locomotion ability. When these conditions were not met, the order of thresholds between successive response categories was skewed, indicating that the rating scale was not being used as anticipated for that particular item (23). Only items with thresholds in the anticipated order were retained.
The third criterion was unidimensionality. The subject’s responses to each item depended only on locomotion ability and not on other patient or item characteristics. Based on the estimated ability of the patient and the estimated difficulty of the item, the expected response of a subject to an item can be computed by the model. The software, through a χ2 fit statistic (24), reports the similarity between the observed and the expected responses to any item. The χ2 fit statistic cumulates the deviations from the model’s expectations. A test of significance is then applied to determine whether the χ2 is too high to be attributed to random variations. If the p-value was less than 0.05, the item did not fit the unidimensionality criterion and was eliminated (25).
The fourth criterion was the Differential Item Functioning (DIF) test (26). This allows verification of the invariance of the scale across different subgroups of children with CP. The score observed for an item should not be influenced by other demographic (e.g. age and sex) or clinical (e.g. type of CP) factors. Hence, children having the same locomotion ability are supposed to obtain the same score on any item, regardless of the other variables. If this is not the case, the item presents a differential functioning.
Three DIF tests were performed on the basis of the following criteria: sex (male vs female), age (≤ 10 vs > 10 years old) and clinical presentation (hemiplegia, diplegia and quadriplegia (27)).
The fifth selection criterion was redundancy. If 2 items had the same level of difficulty and were therefore redundant, the activity with the best fit to the unidimensionality criterion (the item with the lowest χ2) was retained.
Reliability
In Rasch theory, the error measure variance is directly computed from the measurement error accompanying each patient’s ability and item difficulty estimates (17, 28). A person separation reliability coefficient was determined to be the ratio between the true measure variance (as expressed by the standard deviation corrected for measurement error) and the observed (true + error) measure variance in the sample (17). Separation can be used to estimate the number of strata that are significantly distinguished within the range of observed patient abilities.
From the 113 children that this study included, 73 participated in a second assessment one month later. The test-retest reliability of the parents’ responses was determined by the intraclass correlation coefficient (29) (ICC). A DIF test was carried out to verify the reproducibility of item hierarchy between the first and the second assessment.
Concurrent validity
The ABILOCO-Kids measures were validated by assessing their relationship with raw scores of the GMFCS using a Spearman correlation coefficient.
RESULTS
The analysis of the children’s responses resulted in a 5-item questionnaire: 10 items were excluded as more than 90% of the children were not able to estimate their difficulty or had not performed that activity in the last 3 months (e.g. going up an escalator alone; taking the train or the underground railway); 18 items showed a disordered rating scale (e.g. striding over an object with the paretic foot first; stepping up a kerb alone); 3 items did not fit a unidimensional scale (e.g. going up stairs putting each foot on the next step; kicking in a ball with the paretic foot); 3 items had a DIF (e.g. going up and down stairs without holding onto the banisters; running on regular and flat ground); and one item was redundant (running on all types of surfaces). Furthermore, one item was eliminated because most of the children rated it “easy” and this item was, therefore, not relevant. The large number of items showing a disordered rating scale indicated that their perception was more dichotomous. Having difficulty with locomotion activities was perceived by the children as either “impossible” or “easy”, with the intermediate category of “difficult” rarely observed.
The analysis of the parents’ responses resulted in a 10-item questionnaire: 7 items were excluded according to the first selection criterion (e.g. taking the train or the underground railway; ice-skating, skate-boarding, roller-skating); 8 items showed a disordered rating scale (e.g. going up and down stairs holding onto the banisters; walking more than 5 m alone, indoors, on flat ground without an assistive device); 8 items did not fit a unidimensional scale (e.g. kicking in a ball with the paretic foot; riding a bike with a stabilizer); 7 items had a DIF (e.g. running on all types of surfaces; striding over an object with the paretic foot first); and one item was redundant. The partial credit model was retained because it allowed us to maintain more items and to discriminate the locomotion ability with a greater resolution than the rating scale model.
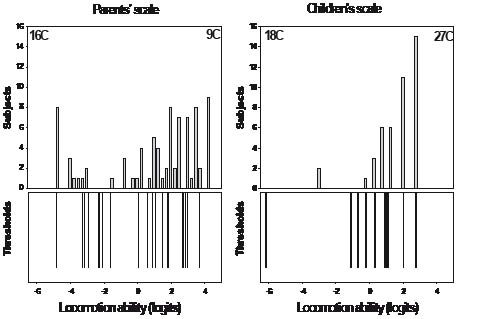
The subjects’ measures and the item threshold distributions for both the parents’ and the children’s scales are presented in Fig. 1. The items are well-targeted on the subjects in both scales. Both scales have a comparable floor effect, but the children’s scale has a greater ceiling effect. Forty-two children with CP considered themselves able to perform all the locomotion activities easily. The parents’ scale covers a wider range of measurements than the children’s scale, indicating a more precise perception of item difficulties. Subjects’ measures are estimated over a range of 9.03 logits by the parents, while they cover 5.70 logits according to the children’s perceptions. Consequently, locomotion ability can be discriminated with a 27 times greater resolution than when using the parents’ perception rather than the children’s.
Fig. 1. Locomotion ability scales as perceived by the parents (10 items, 20 thresholds, left panel) and by the children (5 items, 10 thresholds, right panel) and the corresponding distribution of the subjects (top panels). The item threshold locations are well-targeted on the subject measures on both scales. The floor and the ceiling effects are denoted by the number of children (C) with extreme scores (minimum or maximum) as indicated in the upper corner of the top panels.
Because it allowed a greater discrimination of the 3-level rating scale and a wider range of measurement, the final version of the ABILOCO-Kids questionnaire was built exclusively on the parents’ perceptions.
The calibration of the final 10-item ABILOCO-Kids scale is presented in Table IV. The items are listed, from top to bottom, in order of decreasing difficulty (range: +2.29 to –4.07 logits). Higher logit values represent more difficult activities that require a greater locomotion ability to be performed successfully. Table IV also shows the standard error (SE) associated with each item difficulty (range: 0.230.37 logits; mean: 0.27 logits) and the fit statistic computed as a χ2. A p-value greater than 0.05 indicates that all 10 items contributed to the definition of a unidimensional measure of locomotion ability in our sample. The calibration of the final 5-item ABILOCO-Kids scale, elaborated following the children’s perception, is presented in Table IV.
| Table IV. ABILOCO-Kids calibration for children with cerebral palsy |
| Items | Difficulty (logits) | SE (logits) | χ2 | p-value |
| Parents’ perception | | | | |
| 1. Going up and down stairs without holding onto the banister | 2.29 | 0.23 | 6.15 | 0.19 |
| 2. Running correctly even if you have to turn | 1.46 | 0.23 | 0.75 | 0.95 |
| 3. Going up an escalator alone | 1.03 | 0.24 | 3.36 | 0.50 |
| 4. Walking while holding a fragile object (such as a full glass) | 0.67 | 0.25 | 3.76 | 0.44 |
| 5. Walking several minutes at the same speed as a healthy child | 0.56 | 0.25 | 5.25 | 0.26 |
| 6. Walking backwards | 0.30 | 0.26 | 3.80 | 0.43 |
| 7. Going down stairs putting each foot on the next step | –0.25 | 0.26 | 4.68 | 0.32 |
| 8. Going up stairs putting each foot on the next step | –0.93 | 0.28 | 3.10 | 0.54 |
| 9. Turning and walking in a narrow space | –1.07 | 0.29 | 0.75 | 0.95 |
| 10. Walking less than 5 metres, indoors, holding onto pieces of furniture | –4.07 | 0.37 | 0.84 | 0.93 |
| Children ‘s perception | | | | |
| 1. Walking while holding a fragile object (such as a full glass) | 0.86 | 0.21 | 0.41 | 0.70 |
| 2. Walking backwards | 0.33 | 0.23 | 0.34 | 0.95 |
| 3. Running correctly even if you have to turn | –0.14 | 0.26 | 0.40 | 0.71 |
| 4. Walking alone outside on all types of surfaces | –0.19 | 0.26 | 0.40 | 0.49 |
| 5. Turning and walking in a narrow space | –0.87 | 0.33 | 0.47 | 0.32 |
| SE: standard error. | | | | |
The ABILOCO-Kids scale and the children’s locomotion abilities are shown in Fig. 2. The distribution of the children’s locomotion abilities is presented in the top panel, ranging from –4.71 to +4.31 logits. This illustrates the wide range of locomotion abilities encountered in this study and explored by the ABILOCO-Kids questionnaire.
The bottom panel of the Fig. 2 illustrates the ogival relationship between the total raw scores ranging from 0 to 20 and the measures of locomotion ability on the linear scale in logits. The middle panel shows the expected response to a given item as a function of the underlying locomotion ability. By comparing the locomotion ability of a given child to the difficulty of each item, it is possible to determine the expected response of the patient to the item. According to the parents’ perceptions, a child with an ability of –1 logit would be able to perform the tenth activity easily, to perform the middle activities (items 4–9) with some difficulty, and would be unable to perform the first 3 items. According to the distribution of the subjects’ locomotion abilities, 19% of the children in our sample were able to perform all the activities easily and 15% were not able to perform any of the 10 ABILOCO-Kids items. The 10 items explore a wide range of locomotion abilities that are well-targeted to our sample. The patient reliability equals 0.97, indicating that 5.7 statistically different levels of ability can be distinguished in this sample (28).
Fig. 2. Top panel: Distribution of locomotion ability measures of children with cerebral palsy as perceived by their parents. Twenty-five children with extreme scores cannot be measured by the scale because all activities were either impossible (16C) or easy (9C). Middle panel: A child’s expected response to each item as a function of the underlying measure of locomotion ability. A locomotion ability of zero is by convention set at the average item difficulty. Bottom panel: Ogival relationship between the ABILOCO-Kids total raw score and the locomotion ability measures expressed in logits on the linear scale.
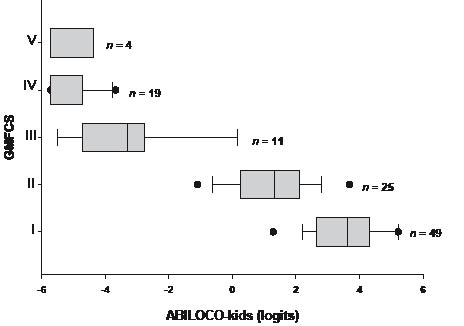
The relationship between ABILOCO-Kids measures and the GMFCS is presented in Fig. 3. The ABILOCO-Kids scores correlated well with the results obtained using the GMFCS (p = –0.88, p < 0.001). On the contrary, the ABILOCO-Kids measures based on children’s perception is not correlated with the GMFCS levels (p = –0.393, p = 0.142). This supports the selection of the parents’ perceptions. A DIF analysis between the children’s and the parents’ perceptions was performed on 10 items from the ABILOCO-Kids questionnaire. Two items presented a DIF between children and parents: “Running correctly even if you have to turn” and “Walking while holding a fragile object (such as a full glass)”.
Fig. 3. Relationship between ABILOCO-Kids measures and Gross Motor Function Classification System (GMFCS) levels. Box plots show the locomotion ability distributions of children with cerebral palsy according to the GMFCS levels: the box indicates the 25% and 75% limits and the vertical line inside the box indicates the median; vertical bars outside the box indicate the 10% and 90% limits; solid dots indicate the 5% and 95% outliers. The number of children (n) in each GMFCS level is indicated.
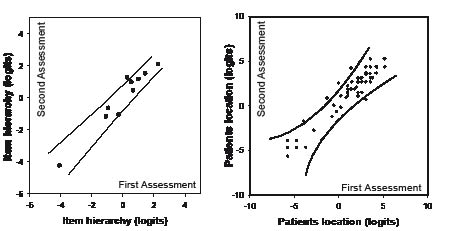
The test-retest reliability (delay: 25 ± 13 days) of the children's measures is shown in Fig. 4 (right panel). Children's locomotion abilities measured at the first and second assessment are highly correlated (ICC = 0.96, p < 0.001). 92% of the measures lie inside the 95% confidence interval (CI) of the identify line, indicating that parents consistently estimate their child’s ability. The left panel shows the DIF plot of the item difficulty hierarchy between the first and the second assessment. The ICC is equal to 0.97 (p < 0.001), indicating a very good reproducibility of the item hierarchy. Nine of the 10 items lie inside the 95% CI of the identity line.
Fig. 4. Left panel: Differential item functioning plot of the item difficulty perceived by the children’s parents at the first and the second assessment (delay: 25 ± 13 days) and the 95% confidence interval (solid line) of the ideal invariance. Nine of the 10 items lie inside the 95% confidence interval. Right panel: relationship between the children’s’ locomotion abilities measured at the first and second assessment and the 95% confidence interval (solid line) of the ideal invariance. Measures (dots) lying within the control lines have the same estimated ability at both the first and the second assessments.
In addition, 5 experts on children with CP were asked to order the 10 items according to difficulty. The similarity in how the items were ordered by the ABILOCO-Kids and by the experts was good (Spearman’s correlation coefficient = 0.78, p < 0.01).
DISCUSSION
This study presents ABILOCO-Kids, a new scale used to measure the walking ability of children with CP that focuses on the ICF Activity domain. A Rasch analysis selected 10 items respecting the principles of linearity, unidimensionality and invariance. The 10 items show a continuous progression in difficulty, are well-targeted to our sample and cover a wide range of functional states. Moreover, the parents evaluate their children consistently after about one month.
The 10-item ABILOCO-Kids questionnaire was built exclusively on parents’ perceptions of their children’s abilities. Indeed, the children’s locomotion ability was better discriminated by the parents than by the children themselves. The questionnaire based on children’s perception presents a great ceiling effect, indicating that the children tended to overestimate their ability. The children also seem to poorly estimate their locomotion ability, as indicated by the absence of a correlation with their GMFCS levels. In addition, the children perceived the activities as either “impossible” or “easy” with very rare intermediate responses. This rather dichotomous perception is consistent with the Piagetian theory in which young children engage in dichotomous thinking (30). The polychotomous perception of the parents provides a more accurate source of information about locomotion ability than the children’s dichotomous perception. Arnould et al. (31) obtained similar results when they developed the ABILHAND-Kids questionnaire to assess manual ability in children with CP. The difference in discrimination between parents and children must be interpreted with some caution, given that a face-to-face interview was used for the children and a written self-report for the parents (31). A written self-administered report is more appropriate for a routine clinical use than a face-to-face interview, which may be influenced by the personality and the style of the interviewer and his/her relationship with the subject (32). Moreover, using the parents’ perception should enable locomotion ability to be assessed in all patients with CP, including very young children and those with mental or communicative disorders.
In comparison with the existing scales, the final 10-item questionnaire (ABILOCO-Kids) presents several advantages. The first is linearity. The Rasch analysis allows the conversion of a total raw score into a linear score that may be submitted to arithmetical computation and parametric statistical analysis. In contrast, the FMS and the FAQ are only ordinal scales that provide a total raw score allowing limited computation. The second advantage is unidimensionality, meaning that ABILOCO-Kids only measures locomotion ability and is not influenced by other child characteristics. The GMFM, the PEDI and the ASK have been analysed following the Rasch model, and therefore respect the concepts of linearity and unidimensionality. However, their latent variable is physical disability and they do not focus on walking ability. Our preliminary questionnaire specifically explored locomotion and included a large number of locomotion activities that a healthy child realizes during his daily life activity and social participation. The third advantage is the invariance of ABILOCO-Kids across sex, age and clinical presentation. The WeeFIM is invariant across age in children older than 3 years of age and the GMFM-66 is invariant across age and disability. Other scales could not be invariant. Indeed, several activities included in the GMFM and the PEDI scales (e.g. stepping up a kerb alone, striding over an object) presented a DIF and were disregarded after the Rasch analysis. ABILOCO-Kids also provides good test-retest reliability. Finally, ABILOCO-kids can be easily incorporated into clinical practice. The parents can complete the questionnaire in the waiting room in just a few minutes. Other questionnaires (PEDI, ASK, WeeFIM and GMFM-66) require a greater amount of time and a skilled staff.
The concurrent validity of ABILOCO-Kids is supported by the correlation between the ABILOCO-Kids results and the GMFCS classification. However, the ABILOCO-Kids questionnaire is more precise. Indeed, 45% of our patients obtained the maximum GMFCS score (Level I), indicating a ceiling effect. Among these patients, the ABILOCO-Kids questionnaire can discriminate a wide range of locomotion ability from 1.07 to 5.22 logits.
The item hierarchy corresponds to the rehabilitation staff experience. The item “walking less than 5 m, indoors, holding onto pieces of furniture” is the easiest activity (item 10) corresponding to the locomotion activity usually acquired first by children (33). Going up and down stairs without holding onto the banister (item 1) requires good balance and sufficient strength in both legs, and is naturally more difficult than going down or up stairs putting each foot on the next step (item 7–8). Running (item 2) requires more stamina and muscular strength than walking. Item 4 “walking while holding a fragile object” requires the ability to perform dual tasks at the same time (34) and requires considerable concentration. The item hierarchy is also related to the clinical presentation. The locomotion ability of the quadriplegic children is distributed from –5.71 to +3.04 logits (mean: –3.54 ± 2.84), of the diplegic children from –4.72 to +4.31 logits (mean: 0.48 ± 3.13), and of the hemiplegic children from –5.71 to +5.22 logits (mean: 2.69 ± 2.35). Thus, on average, the hemiplegic children have greater locomotion ability than the diplegic children, and diplegic children have greater locomotion ability than the quadriplegic children. Furthermore, according to their parents, 15% of the children with CP were not able to perform at least one item, and 94% of these children are quadriplegic. Similarly, the 19% of the children with CP who were able to perform all items easily are all hemiplegic or diplegic.
Tests measuring walking speed in a hospital environment are useful and well validated (35). These tests provide continuous results that can be submitted to parametric statistics, and they have a greater responsiveness than ordinal scales. However, this walking speed test describes a child’s performance under a particular set of circumstances and may not reflect locomotion ability under different conditions. The ABILOCO-Kids is, therefore, complementary to the walking test. Both tests can be performed easily in only a few minutes; the ABILOCO-Kids can also be self-administered. Our questionnaire is also complementary to instrumented gait analysis.
Initially, we hoped to develop a questionnaire that was adapted to assess locomotion ability among children and adults with brain lesions. This is why we selected both adult and children’s activities. The preliminary questionnaire was submitted to 113 children with CP and to 100 adult patients after stroke. Rasch analysis revealed different item selection, calibration and item functioning between adults and children. It was then impossible to build a similar scale adapted to both adult stroke patients and to children with CP. The 13-item questionnaire assessing locomotion ability in stroke patients is presented as ABILOCO (36).
From a practical point of view, whenever a clinician wants to assess the locomotion ability of a child with CP, he asks the parents to complete the ABILOCO-Kids questionnaire. The parents are asked to estimate the child’s ability to perform each of the 10 ABILOCO-Kids activities as “Impossible”, “Difficult” or “Easy”. The activities not attempted by the child within the last 3 months are not scored and are considered as not applicable. The activities that the child does not perform because they are too difficult are scored as “Impossible”. This assessment can be done during a regular consultation to assess the evolution of the child’s locomotion ability as a function of growth. This can also be done before and after a therapeutic intervention (e.g. orthopaedic surgery, botulinum toxin injection or orthosis), in clinical practice or in a research protocol. A website (www.rehab-scales.org) is accessible to perform online analyses to convert total raw scores into linear measures expressed in logits.
In conclusion, ABILOCO-Kids is a questionnaire that assesses the walking ability of children with CP, focusing on the ICF Activity domain. Elaborated following a Rasch analysis, this scale presents good psychometric qualities (reliability, linearity, unidimensionality, invariance and reproducibility). Its responsiveness should be tested in the future.
ACKNOWLEDGEMENTS
The authors thank the Centre Arthur Regniers, the Centre Belge d’Education Thérapeutique pour Infirmes Moteurs Cérébraux (CBIMC), the Centre d’Enseignement et de Traitements Différenciés (CETD), the Coordination de Thérapeutiques pour Handicapés (Cothan), the Ecole Communale “Les Carrefours”, the Fondation Arnaud Fraiteur (FAF), and the Physical Medicine and Rehabilitation department of the Cliniques universitaires Saint-Luc for allowing them to contact and evaluate children with cerebral palsy and their parents.
REFERENCES
1. Rosenbaum PL. Cerebral palsy: what parents and doctors want to know. BMJ 2003; 326: 970–974.
2. World Health Organization. The International Classification of Functioning, Disability and Health-ICF. Geneva: WHO; 2001.
3. Patrick JH, Roberts AP, Cole GF. Therapeutic choices in the locomotor management of the child with cerebral palsy-more luck than judgment? Arch Dis Child 2001; 85: 275–279.
4. Gormley ME Jr, Krach LE, Piccini L. Spasticity management in the child with spastic quadriplegia. Eur J Neurol 2001; 8: 127–135.
5. Butler PB, Thompson N, Major RE. Improvement in walking performance of children with cerebral palsy: preliminary results. Dev Med Child Neurol 1992; 34: 567–576.
6. Nene AV, Evans GA, Patrick JH. Simultaneous multiple operations for spastic diplegia. Outcome and functional assessment of walking in 18 patients. J Bone Joint Surg Br 1993; 75: 488–494.
7. Kuban KCK, Leviton A. Cerebral palsy. N Engl J Med 1994; 330: 188–195.
8. Young NL, Yoshida KK, Williams JI, Bombardier C, Wright JG. The role of children in reporting their physical disability. Arch Phys Med Rehab 1995; 76: 913–918.
9. Russell D, Rosenbaum P, Cadman DT, Gowland C, Hardy S, Jarvis S. The gross motor function measure: a means to evaluate the effects of physical therapy. Dev Med Child Neurol 1989; 31: 341–352.
10. Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Gross motor function classification system for cerebral palsy. Dev Med Child Neurol 1997; 39: 214–223.
11. Haley SM, Coster WJ, Ludlow LH, Haltiwanger JT, Andrellos PJ, editors. Pediatric Evaluation of Disability Inventory (PEDI). Development, standardization, and administration manual, version 1.0. Boston, MA: New England Medical Centre Hospitals; 1992.
12. Young NL, Williams JI, Yoshida KK, Wright JG. Measurement properties of the Activities Scale for Kids. J Clin Epidemiol 2000; 53: 125–137.
13. Ottenbacker KJ, Msall MD, Lyon RN, Granger CV, Braun SB, Feidler RC, et al. The WeeFIM instrument: It’s utility in detecting change in children with developmental disabilities. Arch Phys Med Rehab 2000; 81: 1317–1326.
14. Graham HK, Harvey A, Rodda J, Nattrass GR, Pirpiris M. The Functional Mobility Scale (FMS). J Pediatr Ortho 2004; 24: 514–520.
15. Novacheck T. Reliability and Validity of the Gillette Functional Assessment Questionnaire as an Outcome Measure in Children with Walking Disabilities. J Pediatr Orthoped 2000; 20: 75–81.
16. Rasch G, editor. Probabilistic models for some intelligence and attainment tests. Chicago: Mesa Press; 1992.
17. Wright BD, Masters GN, editors. Rating scale analysis. Chicago: Mesa Press; 1982.
18. Merbitz C, Morris J, Grip JC. Ordinal scales and foundations of misinference. Arch Phys Med Rehab 1989; 70: 308–312.
19. Wright BD, Linacre JM. Observations are always ordinal; measurements, however, must be interval. Arch Phys Med Rehab 1989; 70: 857–860.
20. DeLuca PA, Davis RB III, Ounpuu S. Alterations in surgical decision making in patients with cerebral palsy based on three-dimensional gait analysis. J Pediatr Orthoped 1997; 17: 607–614.
21. Vogels T, Verrips GH, Verloove-Vanhorick SP. Measuring health-related quality of life in children: the development of the TACQOL parent form. Qual Life Res 1998; 7: 457–465.
22. Mutch L. Cerebral palsy epidemiology: where are we now and where are we going? Dev Med Child Neurol 1992; 34: 547–551.
23. Andrich D. Category ordering and their utility. Rasch Meas Transact 1996; 9: 464–465.
24. Andrich D, Sheridan BE, editors. Interpreting RUMM 2020: Part II, Polytomous data. Third edition. Perth, WA: RUMM Laboratory Pty Ltd; 2005.
25. Smith RM, Schumacker RE, Bush MJ. Using item mean squares to evaluate fit to the Rasch model. J Outcome Meas 1998; 2: 66–78.
26. Holland PH, Wainer H. Differential Item Functioning. Hillsdale: Lawrence Erlbaum; 1993
27. Stanley F, Blair E, Alberman E, editors. Clinics in developmental medicine no. 151. Cerebral Palsies: epidemiology and causal pathways. London: Mac Keith Press; 2000.
28. Fisher WP. Reliability statistics. Rasch Meas Transact 1992; 6: 238.
29. Shrout PE, Fleis JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull 1979; 86: 420–428.
30. Chambers CT, Johnston C. Developmental differences in children’s use of rating scales. J Pediatr Psychol 2002; 27: 27–36.
31. Arnould C, Penta M, Renders A, Thonnard JL. ABILHAND-Kids: a measure of manual ability in children with cerebral palsy. Neurology 2004; 63: 1045–1052.
32. Verrips GHW, Stuifbergen MC, den Ouden AL. Measuring health status using the Health Utilities Index: agreement between raters and between modalities of administration. J Clin Epidemiol 2001; 54: 475–481.
33. Woollacott MH, Assaiante C, Amblard B. Development of balance and gait control. In: Bronstein MA, Brandt T, Woollacott MH, Nutt JG, editors. Clinical disorders of balance, posture and gait. 2nd edn. London: Arnold; 2004, p. 39–59.
34. Bowen A. Dual-task effects of talking while walking on velocity and balance following a stroke. Age Ageing 2001; 30: 319–323.
35. Mc Dowell BC, Kerr C, Parkes J, Cosgrove A. Validity of a 1 minute walk test for children with cerebral palsy. Dev Med Child Neurol 2005; 47: 744–748.
36. Caty GD, Arnould C, Stoquart GG, Thonnard JL, Lejeune TM. ABILOCO: a Rasch-built 13-item questionnaire to assess locomotion in stroke patients. Arch Phys Med Rehabil 2008; 89: 284–290.