OBJECTIVE: To investigate changes in arm hand skilled performance during and after active rehabilitation in (sub)groups of subjects with cervical spinal cord injuries.
DESIGN: Longitudinal multi-centre cohort study.
Patients: Persons with cervical spinal cord injuries during (n = 57) and after (n = 35) rehabilitation.
METHODS: Patients from 8 Dutch rehabilitation centres received therapy as usual. At 3 time-points during active rehabilitation and one year after discharge arm hand skilled performance was measured using the Van Lieshout hand function test, the Grasp Release Test (for basic activities) and the Functional Independence Measure and the Quadriplegia Index of Function (for complex activities).
RESULTS: Arm hand skilled performance continues to improve over the entire rehabilitation period, mostly in the first stage of active rehabilitation, and especially in persons with a motor incomplete lesion. Persons with a motor incomplete lesion achieve higher arm hand skilled performance outcome than those with a motor complete lesion. After rehabilitation arm hand skilled performance does not decline.
CONCLUSION: Monitoring the outcome of arm hand skilled performance at the level of basic and complex activities during the whole rehabilitation phase may guide therapists in further optimizing therapy.
Key words: tetraplegia, rehabilitation outcome, upper extremity, skills.
J Rehabil Med 2008; 40: 637–644
Correspondence address: Annemie I. F. Spooren, Zandbergsweg 111, NL-6432 CC Hoensbroek, The Netherlands. E-mail: aspooren@mail.phl.be
Submitted June 14, 2007; accepted April 2, 2008
Introduction
In persons with a cervical spinal cord injury (C-SCI) arm and hand impairments play a major role in the rehabilitation (1–3) and, for the greater part, determine the level of functioning (4). According to the International Classification of Functioning, Disability and Health (ICF), “functioning” can be described on the level of: (i) structure and function, (ii) activity, and (iii) participation (5). As the level of activities includes a broad range of activities of different complexity, a distinction can be made between basic activities, such as grasping and moving objects, and complex activities, such as dressing and grooming. In the present study, the term “arm hand function”’ (AHF) refers to the ICF “function” level, whereas the term “arm hand skilled performance” (AHSP) or upper extremity skilled performance refers to the “activity” level in accordance with the ICF nomenclature.
In order to establish a good rehabilitation policy, insight into the functional deficits, recovery process and rehabilitation outcome is necessary. Information about outcome and the recovery process of the arm and hand at the level of activities is also important because persons with C-SCI expect a better quality of life if their AHSP improves (1–3, 6) and because patients want to know what they will be able to do with their arm and hand.
Most outcome studies in persons with C-SCI describe recovery and outcome of the upper extremity at the level of function, such as neurological recovery (7–11) and recovery of muscle power (12–14), but less has been reported about the recovery and outcome at the activity level. Only a few outcome studies described AHSP on the level of “complex” activities, such as self-care and mobility skills, measured by, for example, the Modified Barthel Index (MBI) (4, 15–18), the Functional Independence Measure (FIMTM) (14, 19, 20) or the Quadriplegia Index of Function (QIF) (21). However, the outcome of these complex activities cannot be attributed to the performance of the arm and hand alone. Outcome at the level of “basic” activities, on the other hand, provides more detailed information concerning what persons with C-SCI are actually able to do with their arm and hand in terms of basic arm skills, such as reaching and fine motor skills. Little has been published on the level of basic activities. Information on the latter level can be obtained by the Van Lieshout Test (VLT) (22–24) and the Grasp Release Test (GRT) (25). The VLT is a new test battery, designed to provide objective information about the quality of the movement of arm and hand. It describes and scores the way the arm and hand is used while performing different skills. The GRT is a quantitative test that expresses how many times a specific task can be performed (26). Harvey et al. (27) described the long-term outcome of the GRT in persons with C-SCI, but this was not a longitudinal study and did not give insight into the development of AHSP.
Because of the small amount of information on AHSP, especially at the level of basic activities, and the importance of AHSP in persons with C-SCI, the present longitudinal study examines the outcome and development of AHSP at the level of basic and complex activities.
The length of inpatient rehabilitation stay varies in different countries, e.g. the length of stay in the Netherlands is, in general, longer than in the USA (28). This should be taken into consideration when comparing outcome at discharge. The present study analyses the outcome of AHSP in 2 stages during active rehabilitation. As some studies report that changes take place after discharge (4, 9, 10, 18, 29), this study will investigate changes in AHSP up to one year after discharge.
Furthermore, as outcome in AHSP is expected to be different depending on the completeness of the lesion (13–15), the present study investigates the outcome of AHSP not only in the total group of patients with C-SCI in general, but also in the persons with a motor complete or motor incomplete C-SCI. To give more detailed information about AHSP within these 2 groups, each of them will be divided into 2 subgroups with either a high or low C-SCI.
The aim of this study is to analyse the changes in AHSP during and after active rehabilitation in persons with C-SCI, and answer the following questions: (i) Is there an improvement in AHSP during and after rehabilitation in persons with a C-SCI? (ii) Is there a difference in progress in AHSP during different stages of rehabilitation and between (sub)groups during (and after) rehabilitation? (iii) Is there a difference in rehabilitation outcome between (sub)groups of persons with a C-SCI during and after rehabilitation?
Methods
Subjects
Eight Dutch rehabilitation centres specialized in the rehabilitation of persons with SCI participated in this programme. Patients with an acute SCI were followed from onset of rehabilitation to one year after discharge.
For the rehabilitation phase, 57 persons with a C-SCI who participated in this longitudinal cohort study were selected. Inclusion criteria were C-SCI (including T1-level), age between 18 and 65 years, performed all tests at the 3 measurement moments during rehabilitation. Exclusion criteria were C-SCI with severe additional neurological, orthopaedic or rheumatological diseases that might interfere with the activities of daily living (ADL) functioning and upper limb skilled performance. For the post-rehabilitation phase, 35 persons with a C-SCI were selected who performed the tests at discharge and at one year after rehabilitation.
Persons were classified by lesion characteristics according to the International Standards for Neurological Classification of Spinal Cord Injury (30). During the upper extremity measurements, the best hand was assessed. Therefore, subjects were categorized by motor level of the best hand at the start of rehabilitation. Patients were also classified as motor complete or motor incomplete according to the American Spinal Injury Association Impairment Scale (AIS) at the start of rehabilitation (30). Different groups were identified: i.e. the total group of persons with a C-SCI (total), persons with a motor complete C-SCI (AIS A or B, (AB group)) and persons with a motor incomplete C-SCI (AIS C or D, (CD group)). Furthermore, the latter 2 groups were divided into 4 subgroups: i.e. persons whose best hand was rated at C5–C6 motor level with an A or B AIS score (high AB); persons whose best hand was rated at C3–C6 motor level with a C or D AIS score (high CD); persons whose best hand was rated at C7–T1 motor level with an A or B AIS score (low AB); and persons with their best hand at C7–T1 motor level with a C or D AIS score (low CD) (30). Persons whose best hand was rated C3–C4 motor level with an AIS C or D score experience upper limb impairment, but are able to perform upper extremity measurements. Therefore these persons were also included in the present study. Persons with a C3–C4 motor level with an AIS A or B score were excluded from the present study, because they were not able to perform activities related to upper extremity measurements.
All subjects gave their informed consent. The protocol of the present study was approved by the medical ethics committee of the Rehabilitation Foundation Limburg and the Institute for Rehabilitation Research in Hoensbroek, the Netherlands.
Procedures
Measurements were conducted by trained research assistants according to a standardized protocol encompassing 3 measurement moments during active rehabilitation. t1 at the start of the active rehabilitation, was defined as the moment subjects were just able to sit in their wheelchair for at least 3 consecutive hours. Patients should be free of their halo or corset. t2 was 3 months later. t3 was at the time of discharge. t4 was the follow-up measurement for the post-rehabilitation phase at one year after discharge.
Measurements
Tests used to measure AHSP at the level of basic activities were the VLT and the GRT. Tests used to measure AHSP at the level of complex activities according to the ICF were the FIMTM and the QIF.
VLT-SF. The VLT (23, 24) assesses the quality of a movement of arm and hand in persons with C-SCI. In the present study the short version or the research version of the VLT (VLT-SF) consisting of 10 items was used. Some items involved basic arm skills, such as forward reaching, other items involved hand and finger skills, such as thumb closure and finger strength. The items pen grip, lighting a match and opening a bottle involved manipulation of objects. Each item has been scored between 0 and 5 for the best hand, whereby score 0 represents that accomplishment of the task was not possible at all and score 5 represents the highest level of performance. The total maximum score was 50. The criterion validity, the inter-rater reliability, the intra-rater reliability and the internal consistency of the VLT-SF were found to be very good (23). The VLT-SF is sensitive to detect changes in AHSP during rehabilitation in people with C-SCI (31).
GRT. In the GRT (25) subjects grasp, move and release 6 different objects as many times as possible in 3 30-second trials for each object. For the present study the average number of successful trials of the best hand was noted for each item and the total score was the sum of the 6 item scores. As the GRT did not have a set maximum score, 200 was considered as a physical limit. This was done after testing people with unimpaired arm hand performance. The GRT was found to be sensitive to change in persons with C-SCI (31).
FIMTM. FIMTM assesses the level of independence of the persons (32). It was found to be useful in detecting changes in functional performance over time in persons with tetraplegia (31, 33). In the present study only the Motor score of the FIM (FIMmot) was used, consisting of 13 items (34). Each item was scored (self-reported) on a 7-point scale varying from total assistance (1) to complete independence (7), resulting in a maximum score of 91.
QIF. QIF is a specific and sensitive instrument to document the functional improvements achieved during the rehabilitation of tetraplegic patients (35) and is able to detect changes in persons with C-SCI during rehabilitation (31). In the current study the short-form QIF was used, which has a high correlation with the long full version of the QIF (36) and consists of 6 ADL. Each item was scored (self-reported) on a 5-point scale (0–4) in order of increasing independence, with a maximum total score of 24. The item “lock the wheelchair” was scored as “independent” if a patient could perform this item or if the person no longer used a wheelchair.
Data analysis
One of the programme partners combined the data into a collective database (www.fbw.vu.nl/onderzoek/A4zon/ZONenglish). The database was verified by checking data with the original forms and by inquiring the research assistants.
To evaluate the progress in AHSP, the median values of the raw scores for each group were used for the 4 different test batteries at the 4 measurement sessions.
A Friedman 2-way analysis of variance by ranks test was used to check whether there was a statistically significant difference in test scores of the VLT, the GRT, the QIF, and the FIMmot across the 3 measurements (t1, t2 and t3). To test in which interval the score had significantly improved during and after rehabilitation, multiple comparison analysis was performed using the Wilcoxon matched-pairs signed-rank test and a Bonferroni correction was applied within each of the 4 test battery conditions. To assess whether there was a significant difference in the amount of improvement between the consecutive intervals, t1–t2 and t2–t3, a Wilcoxon matched-pairs signed rank test was used. To identify statistically significant differences in the amount of progress and in the outcome of AHSP between groups during and after rehabilitation, a Mann-Whitney U-test was used. The level of significance was set at α < 0.05.
Results
Subjects
Group composition, including mean time between date of injury and date of measurements, are presented in Table I. Of the 57 participants in the rehabilitation phase, 34 were also included in the post-rehabilitation phase. One person who was not included in the rehabilitation phase, because of a missing t2 measurement, did participate in the post-rehabilitation phase. The number of participants in the post-rehabilitation phase was lower because subjects were no longer interested or refused to participate (n = 11), were not yet discharged (n = 4), moved abroad (n = 4), had died or developed additional medical problems (n = 2) or for other logistical reasons (n = 2).
| Table I. Population and mean times of measurements |
| | Rehabilitation | Post-rehabilitation |
| n | % | n | % |
| Total population | 57 | 100 | 35 | 100 |
| Male | 45 | 79 | 27 | 77 |
| Female | 12 | 21 | 8 | 23 |
| AB | 32 | 56 | 22 | 63 |
| CD | 25 | 44 | 13 | 37 |
| High AB | 21 | 37 | 14 | 40 |
| High CD | 20 | 35 | 11 | 31 |
| Low AB | 11 | 19 | 8 | 23 |
| Low CD | 5 | 9 | 2 | 6 |
| | Mean | Range | Mean | Range |
| Age (years) at injury | 38 | 18–64 | 35 | 18–56 |
| Days from injury to t1 | 117 | 20–308 | | |
| Days from injury to t2 | 195 | 46–404 | | |
| Days from injury to t3 | 396 | 129–819 | | |
| Days from injury to t4 | | | 836 | 474–1210 |
| Days from t3 to t4 | | | 402 | 278–616 |
| AB (C-SCI with AIS (Asia Impairment Scale) A or B); CD (C-SCI with AIS C or D); high AB (C5–C6 SCI with AIS A or B); high CD (C3–C6 SCI with AIS C or D); low AB (C7–T1 SCI with AIS A or B); low CD (C7–T1 SCI with AIS C or D). t1: start of active rehabilitation; t2: 3 months after t1; t3: at discharge; t4: one year after discharge. |
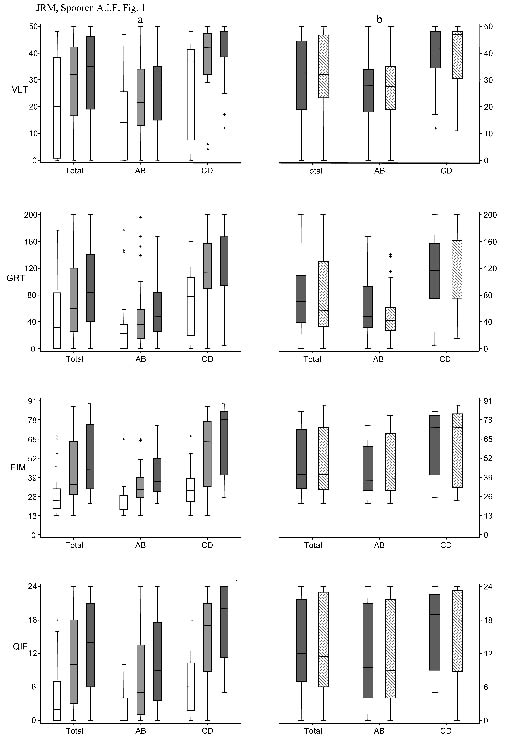
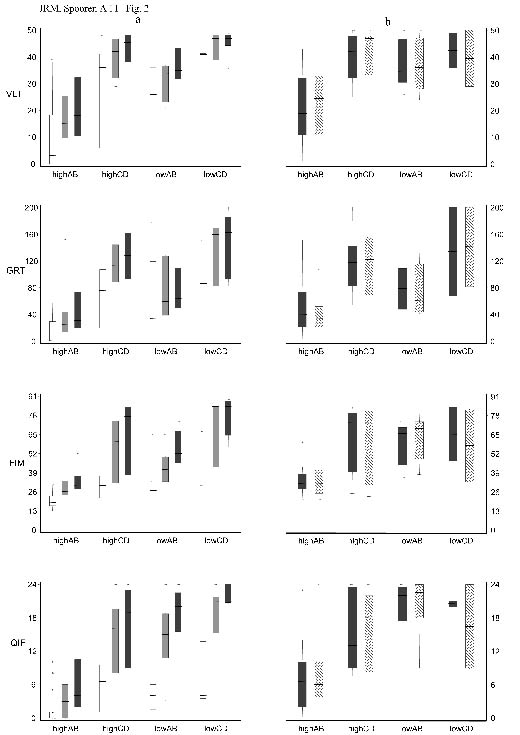
Outcome
Medians, interquartile ranges of the VLT, GRT, FIMmot and QIF scores for the total, the AB and the CD group at t1, t2 and t3 are presented in Fig. 1a and at t3 and t4 in Fig. 1b. Medians, interquartile ranges of the VLT, GRT, FIMmot and QIF scores during and after rehabilitation for both the high and both the low subgroups are presented in Fig. 2a and 2b.
Fig. 1. Outcome measures of arm hand skilled performance (AHSP) (a) during rehabilitation and (b) after rehabilitation for total group, AB and CD group. VLT (Van Lieshout Test), GRT (Grasp Release Test), FIM (Functional Independence Measure, motor), QIF (Quadriplegia Index of Function). X-axis: total (total group of persons with C-SCI); AB (C-SCI with AIS (Asia Impairment Scale) A or B); CD (C-SCI with AIS C or D).
: t1 (start of active rehabilitation); : t2 (3 months after t1); : t3 (at discharge); : t4 (one year after discharge).
Fig. 2. Outcome measures of arm hand skilled performance (AHSP) (a) during rehabilitation and (b) after rehabilitation for 4 groups: high AB, high CD, low AB and low CD group. VLT (Van Lieshout Test), GRT (Grasp Release Test), FIM (Functional Independence Measure, motor), QIF (Quadriplegia Index of Function). X-axis: high AB (C5-C6 SCI with AIS (Asia Impairment Scale) A or B); high CD (C3-C6 SCI with AIS C or D); low AB (C7-T1 SCI with AIS A or B); low CD (C7-T1 SCI with AIS C or D).
: t1 (start of active rehabilitation); : t2 (3 months after t1); : t3 (at discharge); : t4 (one year after discharge).
Active rehabilitation phase
The total, the AB and the CD groups demonstrate an improvement in AHSP, as measured by all test batteries used, across the 3 measurements (Friedman, p < 0.001). This improvement can be seen in the first and second stages of rehabilitation (p < 0.001). Comparing the amount of improvement in AHSP between intervals, the total and the CD group demonstrate more improvement in the first interval than in the second on all test batteries used (p < 0.005). For the AB group the amount of improvement between intervals was less pronounced. Only the VLT demonstrates statistically more improvement in the first interval than in the second (p < 0.05). These findings were corroborated by the fact that the CD group makes more progress than the AB group in the first interval, as measured by all test batteries used (p < 0.005), except for the VLT. At the end of rehabilitation, the CD group achieves a higher outcome than the AB group on AHSP, as measured by all test batteries used (p < 0.003).
For persons with a high C-SCI similar findings are observed as in the total groups (see Fig. 2a). For persons with a low C-SCI, an improvement in AHSP can be seen on all test batteries used between t1 and t2, however this was only statistically significant for the low AB group (p < 0.01). In the second interval, the low AB group demonstrates an improvement on the QIF and the FIMmot (p < 0.01).
Post-rehabilitation phase
Fig. 1b shows only minor changes in AHSP. Note that the t3 values of the rehabilitation phase (Fig. 1a) and of the post-rehabilitation phase (Fig. 1b) are different group compositions. Although the AB group demonstrates a small increase on the FIMmot, the improvement was statistically significant (p < 0.05). Comparing the amount of improvement between groups, the AB group demonstrates statistically significantly more progress on the FIMmot than the CD group (p < 0.01). The outcome on AHSP at t4 was higher for the CD group than for the AB group and this was statistically corroborated for the GRT and the VLT (p < 0.05).
For the high C-SCI subgroups, findings are similar to those of the total group (see Fig. 2b). There are, however, a few differences: the changes on the FIMmot are very small, the high CD group demonstrates an increase in the median QIF, whereas the total group demonstrates a slight decrease and the outcome of the FIMmot at t4 is additionally to the GRT and the VLT statistically significantly higher for the CD group than for the AB group (p < 0.05). The low AB group demonstrates significant progress on the FIMmot (p < 0.018), as in the total AB group, and makes statistically more progress on the FIMmot than the low CD group (p < 0.05), which demonstrates a decrease in the FIMmot.
Discussion
The aim of the present study was to analyse changes in AHSP during and after rehabilitation in (sub)groups of persons with a C-SCI.
Improvement in AHSP during and after rehabilitation
In general, all persons with C-SCI improve with regard to arm hand skilled performance on the level of basic and complex activities during the 2 stages of active rehabilitation. Post-rehabilitation, changes in AHSP are very small. No decline in AHSP was observed.
It was expected that AHSP would improve in the first stage of rehabilitation, as described in earlier reports stating that improvement in general skills and neurological recovery takes place in the initial phase of the rehabilitation (9, 10, 13, 15). As to the second rehabilitation stage, less progress was expected (4, 8–10). In contrast, the present study revealed significant improvement in AHSP. This is even more remarkable as the second stage of the present study started at on average 195 days post-injury, because of late onset of intensive active training due to patients wearing a halo or corset and patients were able to sit for 3 consecutive hours. In the study of Yarkony et al. (15) tetraplegic patients were already discharged at (on average) 121 days post-injury. Similar data were found in several other outcome studies in the USA (4, 28).
The fact that significant changes in AHSP are observed a long time after the injury gives rise to 2 considerations. The first is to what extent the improvement in AHSP is influenced by neurological recovery or by active rehabilitation. Yarkony et al. (15) reported that functional improvement occurs most rapidly during inpatient rehabilitation, attributing this effect to the combination of neurological recovery, intensity of training and multidisciplinary approach. Furthermore, Burns & Ditunno (8) and Waters et al. (9, 10) described that most neurological recovery occurs in the first 6 months after injury, with the highest speed of recovery in the first 3–6 months. As in the present study, inpatient rehabilitation was longer and the start of active training was later than in earlier mentioned USA studies, possible effects of spontaneous recovery might have been less, especially in the latter part of the rehabilitation phase. This will be studied in future research. As the start of the active rehabilitation in the present study was later, it is conceivable that functional improvement on AHSP might occur at a later stage. On the other hand, it might also be possible that improvement in AHSP carries on longer, because of the longer inpatient stay. Post et al. (28), for example, found a slightly better functional outcome in persons with tetraplegia in the Netherlands compared with the USA. Further research is needed to assess the influence of these factors on the outcome of AHSP. The second consideration is that the present study investigated changes in AHSP, whereas other outcome studies looked at more general skills, as measured by the MBI (4, 15–18), or at neurological recovery (13). One could argue that the recovery of AHSP carries on longer than general functional skills and neurological recovery. On the other hand, it might also be possible that the test batteries used in the present study are more sensitive to detect the small changes in AHSP, in contrast to those used in other studies.
After rehabilitation, only weak changes in AHSP were expected because of the rather small number of patients participating in the post-rehabilitation phase and because of evidence from earlier research that improvement after discharge is very limited and slow (11, 14, 29). The present study showed that the level of AHSP does not decline post-discharge. However, data from larger groups is required to make more detailed inferences.
Difference in progress of AHSP between stages of the rehabilitation and between groups
In general, it can be concluded that more progress in AHSP is made during the first stage of rehabilitation than during the second stage and this is more pronounced in persons with a motor incomplete lesion. The latter can be attributed to the training capacities of persons in the first stage of rehabilitation. Persons with an incomplete lesion have more residual function and a greater potential, i.e. the larger possibilities to compensate function loss, and may take a quicker start in rehabilitation. As most neurological recovery takes place in the first 6 months after injury (8–10), most recovery in functional outcome is also expected in the first stage of rehabilitation. Our findings are also in accordance with findings of Ditunno et al. (13, 14) who reported that persons with an incomplete lesion reach a plateau earlier than those with a complete lesion.
In persons with a motor complete lesion the difference in progress between the first and second stage was less pronounced, except for the basic activities. Basic activities, which involve more isolated movements of body parts, may be easier to train and perform at the beginning of the rehabilitation, especially for persons with a complete lesion. Complex activities, on the other hand, involve whole body movement, such as transfers and other gross motor daily activities, and will be trained later in the rehabilitation in persons with less residual capacity, such as persons with a complete lesion. This explanation is in accordance with our finding that the differences in progress in AHSP between the complete and the incomplete group is more pronounced in the first interval for the complex activities.
Although differences in progress between groups after rehabilitation are very small, progress of the FIM, in which persons with a complete lesion demonstrate an increase and persons with an incomplete lesion a slight decrease, is statistically significant. However, different and small group sizes and within-group variability limit further conclusions.
Difference in rehabilitation outcome of AHSP between motor complete and motor incomplete groups
Taking into account the differences in amount of improvement, it can be concluded that at the end of the rehabilitation phase, persons with a motor incomplete lesion reach a higher outcome than those with a motor complete lesion. This is in accordance with other studies on outcome and recovery, which reported that persons with an incomplete C-SCI attained a higher outcome on neurological recovery, on upper extremity strength and a higher FIMTM score (7, 13, 15, 20, 29, 37). After rehabilitation, persons with an incomplete lesion achieve a higher outcome on AHSP than those with a motor complete lesion. The fact that statistically this was corroborated only by the VLT and the GRT might be attributed to the larger interquartile ranges of the data on complex activities.
Methodological considerations and future research
There are some limitations to the present study. It included 57 persons in the rehabilitation phase and 35 in the post-rehabilitation phase. One might argue that these groups are not very large. However, they are a good representation of the total C-SCI population in the Dutch rehabilitation centres specialized in SCI treatment. A small number of persons with a C-SCI were excluded from the programme for various reasons, i.e. progressive diseases, psychological problems, language problems or refusing to participate in the programme. Also the post-rehabilitation group is representative: the only difference with the rehabilitation group was the smaller percentage of persons with an incomplete lesion. To give more detailed information on lesion level, the groups were divided into subgroups, which sometimes resulted in very small groups (e.g. especially the low C-SCI motor incomplete group in the post-rehabilitation phase). Analyses were also performed after splitting the C3–C6 CD group into C3–C4 CD and C5–C6 CD subgroups, but this did not provide additional information. To obtain more detailed information about each lesion level, more data need to be gathered. Another restriction was that only the best hand was measured for the VLT and the GRT. As a consequence, some people did not make much progress, because they had almost reached the maximum score with their best hand. Other people were excluded because their “best hand” was unimpaired. Some data show large interquartile ranges, indicating that variance is somewhat high. This might reduce when assessing a larger sample. Nevertheless, progress still remained statistically significant, with exception in the post-rehabilitation phase, indicating variance was less of a problem in this study. On the other hand, a lack of statistical significance because of high variance does not necessarily mean that there is no clinically meaningful change.
When interpreting the results of the FIMTM and the QIF, one should bear in mind that these complex activities are not solely influenced by arm and hand, but also by the whole body (31), especially in persons with an incomplete lesion.
Most studies described the total group of tetraplegic persons, making a distinction at the level of completeness, i.e. complete (AIS A) group vs the incomplete (AIS B, C and D) group (4, 9, 10, 15). In the present study, the motor complete (AIS A and B) vs the motor incomplete (AIS C and D) group was described, which was also done by Ditunno et al. (13). This division is justified as most neurological recovery takes place in the first 6 months after injury with the highest rate of recovery in the first 3 months (29) and the t1 measurement in the present study was at a mean of 117 days (± 4 months) after injury.
The present study demonstrates that improvement of AHSP carries on longer than improvement in AHF and general functional skills, as described in other studies. However, the inpatient stay is different in the present study. Future research should examine the impact of length of stay, of period of inpatient rehabilitation and the impact of intensity and type of training on outcome of AHSP. Furthermore, future research should assess whether neurological recovery and changes in AHF are related to changes in AHSP.
Monitoring the outcome of AHSP at the level of complex and basic activities may guide therapists in further optimizing therapy. Furthermore, one should realize that the evolution of AHSP may vary in relation to the rehabilitation conditions. However, (para)medical staff should be aware of patients’ potential so as to maximize functional outcome even after discharge, especially when patients are discharged early.
Acknowledgements
This study is part of the ZONMW Rehabilitation Research programme “Physical strain, work capacity and mechanisms of restoration of mobility in the rehabilitation of individuals with spinal cord injury” and was funded through grant 1450010. The PHL University College, department of Health Care, Belgium, provided additional funds.
References
1. Hanson RW, Franklin MR. Sexual loss in relation to other functional losses for spinal cord injured males. Arch Phys Med Rehabil 1976; 57: 291–293.
2. Snoek GJ, IJzerman MJ, Hermens HJ, Maxwell D, Biering-Sorensen F. Survey of the needs of patients with spinal cord injury: impact and priority for improvement in hand function in tetraplegics. Spinal Cord 2004; 42: 526–532.
3. Welch RD, Lobley SJ, O’Sullivan SB, Freed MM. Functional independence in quadriplegia: critical levels. Arch Phys Med Rehabil 1986; 67: 235–240.
4. Yarkony GM, Roth EJ, Heinemann AW, Lovell L, Wu YC. Functional skills after spinal cord injury rehabilitation: three-year longitudinal follow-up. Arch Phys Med Rehabil 1988; 69: 111–114.
5. World Health Organization. ICF: International classification of functioning, disability and health. Geneva: World Health Organisation; 2001.
6. McDowell CL, Rago TA, Gonzalez SM. Tetraplegia. Hand Clin 1989; 5: 343–348.
7. Marino RJ, Ditunno JF Jr, Donovan WH, Maynard F Jr. Neurologic recovery after traumatic spinal cord injury: data from the Model Spinal Cord Injury Systems. Arch Phys Med Rehabil 1999; 80: 1391–1396.
8. Burns AS, Ditunno JF. Establishing prognosis and maximizing functional outcomes after spinal cord injury: a review of current and future directions in rehabilitation management. Spine 2001; 26 Suppl 24: S137–S145.
9. Waters RL, Adkins RH, Yakura JS, Sie I. Motor and sensory recovery following complete tetraplegia. Arch Phys Med Rehabil 1993; 74: 242–247.
10. Waters RL, Adkins RH, Yakura JS, Sie I. Motor and sensory recovery following incomplete tetraplegia. Arch Phys Med Rehabil 1994; 75: 306–311.
11. Kirshblum S, Millis S, McKinley W, Tulsky D. Late neurologic recovery after traumatic spinal cord injury. Arch Phys Med Rehabil 2004; 85: 1811–1817.
12. Fujiwara T, Hara Y, Akaboshi K, Chino N. Relationship between shoulder muscle strength and functional independence measure (FIM) score among C6 tetraplegics. Spinal Cord 1999; 37: 58–61.
13. Ditunno JF Jr., Cohen ME, Hauck WW, Jackson AB, Sipski ML. Recovery of upper-extremity strength in complete and incomplete tetraplegia: a multicenter study. Arch Phys Med Rehabil 2000; 81: 389–393.
14. Ditunno JF, Burns AS, Marino RJ. Neurological and functional capacity outcome measures: Essential to spinal cord injury clinical trials. J Rehabil Res Dev 2005; 42 Suppl 1: 35–42.
15. Yarkony GM, Roth EJ, Heinemann AW, Wu YC, Katz RT, Lovell L. Benefits of rehabilitation for traumatic spinal cord injury. Multivariate analysis in 711 patients. Arch Neurol 1987; 44: 93–96.
16. Schonherr MC, Groothoff JW, Mulder GA, Eisma WH. Functional outcome of patients with spinal cord injury: rehabilitation outcome study. Clin Rehabil 1999; 13: 457–463.
17. Granger CV, Albrecht GL, Hamilton BB. Outcome of comprehensive medical rehabilitation: measurement by PULSES profile and the Barthel Index. Arch Phys Med Rehabil 1979; 60: 145–154.
18. Dzidic I, Moslavac S. Functional skills after the rehabilitation of spinal cord injury patients; observation period of 3 years. Spinal Cord 1997; 35: 620–623.
19. Muslumanoglu L, Aki S, Ozturk Y, Soy D, Filiz M, Karan A, et al. Motor, sensory and functional recovery in patients with spinal cord lesions. Spinal Cord 1997; 35: 386–389.
20. Ota T, Akaboshi K, Nagata M, Sonoda S, Domen K, Seki M, et al. Functional assessment of patients with spinal cord injury: measured by the motor score and the Functional Independence Measure. Spinal Cord 1996; 34: 531–535.
21. Yavuz N, Tezyurek M, Akyuz M. A comparison of two functional tests in quadriplegia: the quadriplegia index of function and the functional independence measure. Spinal Cord 1998; 36: 832–837.
22. Lieshout GV, editor. User manual Van Lieshout Test. Hoensbroek: iRv; 2003.
23. Post MW, Van Lieshout G, Seelen HA, Snoek GJ, Ijzerman MJ, Pons C. Measurement properties of the short version of the Van Lieshout test for arm/hand function of persons with tetraplegia after spinal cord injury. Spinal Cord 2006; 44: 763–771.
24. Post MWM, editor. Pilot-onderzoek Van Lieshout Test. Hoensbroek [The Van Lieshout Test: a pilot study]: iRv; 2000. (in Dutch).
25. Stroh Wuolle K, van Doren CL, Thrope GB, Keith MW, Peckham PH. Development of a quantitative Hand Grasp and Release Test for patients with tetraplegia using a hand neuroprosthesis. J Hand Surg 1994; 19A: 209–218.
26. Mulcahey MJ, Smith BT, Betz RR, Weiss AA. Outcomes of tendon transfer surgery and occupational therapy in a child with tetraplegia secondary to spinal cord injury. Am J Occup Ther 1995; 49: 607–617.
27. Harvey LA, Batty J, Jones R, Crosbie J. Hand function of C6 and C7 tetraplegics 1–16 years following injury. Spinal Cord 2001; 39: 37–43.
28. Post MW, Dallmeijer AJ, Angenot EL, van Asbeck FW, van der Woude LH. Duration and functional outcome of spinal cord injury rehabilitation in the Netherlands. J Rehabil Res Dev 2005; 42 Suppl 1: 75–86.
29. Kirshblum SC, O’Connor KC. Predicting neurologic recovery in traumatic cervical spinal cord injury. Arch Phys Med Rehabil 1998; 79: 1456–1466.
30. Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE, et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003; 26 Suppl 1: S50–S56.
31. Spooren AI, Janssen-Potten YJ, Post MW, Kerckhofs E, Nene A, Seelen HA. Measuring change in arm hand skilled performance in persons with a cervical spinal cord injury: responsiveness of the Van Lieshout Test. Spinal Cord 2006; 44: 772–779.
32. Hamilton BB, Laughlin JA, Granger CV, Kayton RM. Interrater Agreement of the Seven Level Functional Independence Measure (FIM). Arch Phys Med Rehabil 1991; 72: 790.
33. Hall KM, Cohen ME, Wright J, Call M, Werner P. Characteristics of the Functional Independence Measure in traumatic spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1471–1476.
34. Linacre JM, Heinemann AW, Wright BD, Granger CV, Hamilton BB. The structure and stability of the Functional Independence Measure. Arch Phys Med Rehabil 1994; 75: 127–132.
35. Gresham GE, Labi ML, Dittmar SS, Hicks JT, Joyce SZ, Stehlik MA. The Quadriplegia Index of Function (QIF): sensitivity and reliability demonstrated in a study of thirty quadriplegic patients. Paraplegia 1986; 24: 38–44.
36. Marino RJ, Goin JE. Development of a short-form Quadriplegia Index of Function scale. Spinal Cord 1999; 37: 289–296.
37. Poynton AR, O’Farrell DA, Shannon F, Murray P, McManus F, Walsh MG. Sparing of sensation to pin prick predicts recovery of a motor segment after injury to the spinal cord. J Bone Joint Surg Br 1997; 79: 952–954.