OBJECTIVE: To assess the effectiveness of a single home visit by an occupational therapist in the reduction of fall risk after hip fracture in elderly women.
DESIGN: Quasi-randomized controlled trial.
PARTICIPANTS: Ninety-five women aged 60 years or older, living in the community, who sustained a fall-related hip fracture.
METHODS: The women were allocated alternately to intervention or control groups. All the women underwent a multidisciplinary programme targeted at fall prevention during in-patient rehabilitation. Additionally, the intervention group received a home visit by an occupational therapist a median of 20 days after discharge. Falls were recorded at a 6-month follow-up.
RESULTS: Thirteen of the 50 women in the control group sustained 20 falls during 9231 days, whereas 6 of the 45 women in the intervention group sustained 9 falls during 8970 days. After adjustment for observation periods, Barthel Index scores, and body height, a significantly lower proportion of fallers was found in the intervention group: the odds ratio was 0.275 (95% confidence interval 0.081–0.937, p = 0.039).
CONCLUSION: A single home visit by an occupational therapist after discharge from a rehabilitation hospital significantly reduced the risk of falling in a sample of elderly women following hip fracture.
Key words: falls, hip fracture, home visit, occupational therapy, rehabilitation.
J Rehabil Med 2008; 40: 446–450
Correspondence address: Marco Di Monaco, Osteoporosis Research Center, Presidio Sanitario San Camillo, Strada Santa Margherita 136, IT-10131 Torino, Italy. E-mail: Medici@h-sancamillo.to.it
Submitted August 22, 2007; accepted February 25, 2008
INTRODUCTION
Approximately 33% of all people over 65 years of age who are living in the community fall each year (1). Falls carry a relevant burden of morbidity and mortality, and it has been estimated that 20% of fall incidents require medical attention (2) and 5–10% cause serious injuries, including major head trauma, major lacerations or bone fractures (3). Even without injury, falls cause a loss of confidence that results in reduced physical activity, increased dependency, and social withdrawal (4). Institutionalization is strongly predicted by previous falls (5). Because various intervention programmes have been shown to reduce the number of fallers among elderly people (2, 6), falls have become a target for public health preventive efforts (7). Effective prevention consists mainly of multifactorial, multidisciplinary programmes based on the search for modifiable risk factors for falls in individual subjects, followed by targeted interventions (8–10). These include physical exercise to improve strength and balance, advice and training on the use of assistive devices, environmental modifications, health education to address home hazards that contribute to falls, and clinical management for optimization of health, including withdrawal of medications that increase fall risk (2, 6).
Nearly all hip fractures in ageing people occur as a result of a fall (11). Hip fracture is a leading cause of mortality and morbidity in the elderly: it is associated with a significant increase in mortality ranging from 10% to 30%, whereas only 40% of hip-fracture survivors fully regain their pre-fracture level of independence, and up to 25% may require long-term nursing-home care (12). Hip-fracture survivors are at high risk for a recurrent fracture on the contralateral side (13). The sequential fracture of both hips is becoming a common condition, because up to 10% of patients with a recent hip fracture actually had a recurrent fracture of the hip in cross-sectional studies (14, 15) and 21% of the patients from a population-based study, who sustained a hip fracture and were aged 85 years or older had suffered at least 2 hip fractures (16). Given the high risk for falls and new fractures, hip-fracture survivors are a target for fall-preventive interventions. However, the implementation of preventive programmes in this group of individuals at high risk is low (17), and few studies have focused on hip-fracture patients (18, 19) with the aim of optimizing fall prevention strategies.
The aim of this study was to assess the role of a post-discharge home visit by an occupational therapist in reducing the risk of falling in a sample of elderly hip-fracture women who received a standard multidisciplinary intervention to prevent falls during their stay in our rehabilitation hospital.
PATIENTS AND METHODS
Recruitment and randomization
The study was performed in Turin, a city of approximately 1 million inhabitants. We assessed for eligibility 270 women aged 60 years or older who were admitted consecutively to our physical medicine and rehabilitation division because of their first hip fracture during a 26-month period. Among the 270 women, only those who fulfilled the following criteria were invited to participate in the study: community-dwelling women, who lived in Turin who planned to return to same dwelling at discharge (non-institutional), whose fractures were due to falls, and whose Mini Mental State Examination test score was higher than 23.
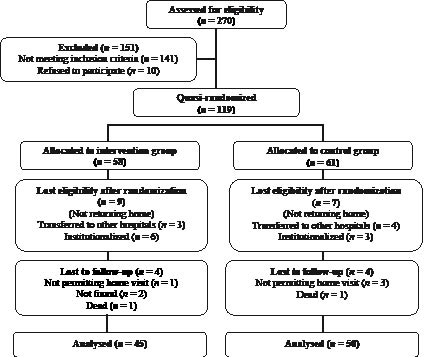
A total of 141 women did not meet the inclusion criteria listed above and were excluded from the study. The remaining 129 women were invited to participate in the study. Ten of these 129 refused. The remaining 119 women were allocated to intervention or control groups alternately. Sixteen of the 119 randomized women were found not to satisfy the entry criteria at the time of discharge from the rehabilitation hospital, because they did not actually return home: 7 women (3 from the intervention group and 4 from the control group) were transferred to other hospitals during their stay in the rehabilitation division because of acute concomitant diseases, whereas 9 women (6 from the intervention group, 3 from the controls) were institutionalized. We were not able to obtain outcome data in 8 of the remaining 103 women: 4 (1 from the intervention group and 3 from the controls) withdrew their consent (they did not permit the pre-planned home visit of the occupational therapist at the end of the follow-up period), 2 (both from the intervention group) were not found, whereas the other 2 (1 from the intervention group and 1 from the controls) died during the follow-up period. Finally, the study sample included 95 women (45 in the intervention group and 50 controls), who completed the study and were included in the analysis. Fig. 1 shows the flow-chart of the trial.
Fig. 1. Trial flow-chart.
Intervention
During their stay in our rehabilitation hospital, all the 95 women received a multidisciplinary intervention to prevent falls, as a part of the usual rehabilitation protocol. The intervention consisted of 1–3 h a day for 5 days a week of physical exercise to improve strength and balance, advice and training on the use of assistive devices, and training in activities of daily living conducted by physiotherapists and occupational therapists. At least 3 h of the stay in the rehabilitation hospital were devoted to a skilled occupational therapist assessing home hazards of falling on the basis of a standard checklist that took into account both the home environment as described by the patients and their caregivers or relatives and behaviour during activities of daily living. The occupational therapist suggested targeted modifications of the home environment and behavioural changes to prevent falls. All the women received a free brochure describing the main rules to prevent falls and underwent a geriatric evaluation for optimization of health. In addition, the geriatrist checked the possibility of withdrawing all the medications in use that are known to increase the risk of falling. All the women were treated with a daily oral supplementation of vitamin D (880 IU) plus calcium (1 g), given its effectiveness in fall prevention (20, 21) and in osteoporosis treatment in elderly subjects (22). We recommended continuing this treatment after discharge from our hospital.
Additionally, the 45 women in the intervention group received a home visit by an occupational therapist at a median of 20 days (interquartile range 11; range 6–44 days) after discharge from our hospital. The occupational therapist assessed environmental hazards, behaviours in activities of daily living, and use of assistive devices and suggested targeted modifications to prevent falls. The home visit took a mean duration of 60 min (range 45–70 min).
Outcome measures
The outcome of interest was the occurrence of falls. We defined a fall as “any event when the participant unexpectedly came to rest on the ground, floor, or another lower level” (23). During their stay in hospital, all the women were asked to record falls occurring after discharge, and to report them at a home visit by an occupational therapist scheduled for approximately 6 months after discharge. During this home visit, the occupational therapist asked the women in detail about falls occurring after discharge from hospital. The time of fall occurrence was not recorded. The level of adherence to the advice given during the first home visit was checked for the women in the intervention group. The percentage of advice followed by each woman was recorded. All outcome assessments were performed by 2 occupational therapists; the same 2 who conducted all the home visits.
As possible confounders, we assessed functional independence in activities of daily living before fracture, on admission to rehabilitation, on discharge from rehabilitation and during the home visit conducted by an occupational therapist at the end of the study, using the Barthel Index score (original version, unchanged) (24). Serum levels of 25-hydroxyvitamin D were assessed during stay in the rehabilitation hospital by immunoenzymatic assay (normal range 9–42 ng/ml; coefficient of variation intra-assay < 8%; inter-assay < 10%) (IDS Inc., Fountain Hills, AZ, USA).
The study was approved by the local Committee for Medical Research (Regione Piemonte) and written informed consent was obtained from participants.
Statistical analysis
Sample size was calculated to detect a 50% decrease in the proportion of fallers with a power of 80% and a 2-sided alpha level of 0.05, given an estimated proportion of fallers of 53% in the control group (25). Descriptive statistics for the 95 women are shown in Table I. We assessed the association between the allocation group and the proportion of fallers using logistic regression. Because the dependent variable was dichotomous (fallers/not fallers), we chose binary logistic regression. Data was adjusted for the period of observation since hospital discharge till the final home visit in both groups. The analyses were repeated adjusting data for the period of observation from the first home visit to the final home visit in the intervention group. Furthermore, we tested the bivariate association between the proportion of fallers and all the variables listed in Table I. For 2 of these variables, i.e. Barthel index scores assessed at the end of in-patient rehabilitation and body height, we found a p-value < 0.30. The 2 variables were included as co-variates together with allocation group and days of observation in the binary logistic regression. The pivotal analysis was performed including all the 95 women who completed the study. In addition, we performed the same analysis in 2 subgroups: we excluded the women in the intervention group who did not follow any advice given during the first home visit conducted by an occupational therapist, or those who did not follow at least 50% of the advice.
The statistical package used was SPSS, version 14 (SPSS, Inc., Chicago, IL, USA).
| Table I. Characteristics of the 2 groups of patients (given as mean and standard deviation where not otherwise stated) |
| | Intervention group (n = 45) | Control group (n = 50) |
| Age (years) | 79.9 (6.4) | 80.1 (6.8) |
| Body weight (kg) | 58.7 (13.7) | 59.2 (11.1) |
| Body height (cm) | 155.2 (6.2) | 155.6 (6.8) |
| Hip-fracture type: trochanteric/cervical (%) | 51/49 | 52/48 |
| Surgical procedure type: arthroplasty/internal fixation (%) | 51/49 | 50/50 |
| Concomitant diseases | 2.7 (1.1) | 2.8 (2.0) |
| Medications in use | 4.3 (1.9) | 4.3 (2.6) |
| 25-hydroxyvitamin D (ng/ml) | 11.0 (8.9) | 13.0 (11.3) |
| Barthel Index score before fracture (median; IQR) | 100 (95–100) | 100 (95–100) |
| Barthel Index score on admission (median; IQR) | 50 (40–60) | 45 (36–56) |
| Barthel Index score on discharge (median; IQR) | 90 (72–95) | 90 (70–95) |
| Length of stay in hospital (days) (median; IQR) | 34 (29–38) | 36 (31–40) |
| Period of observation (days) (median; IQR) | 195 (177–211) | 183 (173–203) |
| Mini Mental State Examination score (median; IQR) | 26 (25–27) | 26 (25–28) |
| IQR: interquartile range. | | |
RESULTS
Thirteen of the 50 women in the control group sustained 20 falls during 9231 days, whereas 6 of the 45 women in the intervention group sustained 9 falls during 8970 days. All the 9 falls recorded in the patients belonging to the intervention group occurred after the first home visit conducted by an occupational therapist. Without adjustments, we did not find a significant difference in the proportion of fallers between the 2 groups: the odds ratio was 0.438 (95% confidence interval (CI) 0.151–1.272; p = 0.129). After adjustment for observation length, Barthel Index scores assessed before the beginning of the observation period, and body height, we found a significantly lower proportion of fallers in the intervention group: the adjusted odds ratio was 0.275 (95% CI 0.081–0.937, p = 0.039). The regression model is shown in Table II. When we substituted the period of observation since the home visit for the period since hospital discharge for the patients in the intervention group the results did not change materially (data not shown). Given the absolute risk of experiencing one or more falls in the control group (13/50 = 26%), and the corresponding odds of 0.351, the adjusted odds and absolute risk for falling in the intervention group were 0.097 and 8.8%, respectively, with a relative risk of 0.34.
| Table II. Logistic regression analysis: factors associated with the proportion of fallers. The dependent variable was the proportion of participants who experienced one or more falls during the observation period (who were conventionally attributed a value of 1, whereas the non-fallers were conventionally attributed a value of 0). The independent variables included in the regression model are listed. The intervention group was conventionally attributed a value of 1 (the control group was attributed a value of 0) |
| | B | Odds ratio and 95% CI | p |
| Allocation group | –1.290 | 0.275 (0.081–0.937) | 0.039 |
| Barthel Index assessed before the beginning of the observation period | –0.031 | 0.969 (0.939–1.000) | 0.051 |
| Period of observation | 0.017 | 1.018 (0.998–1.037) | 0.078 |
| Body height | 0.059 | 1.061 (0.980–1.148) | 0.142 |
| CI: confidence interval. | | | |
A mean of 3.9 (standard deviation (SD) 2.5) pieces of advice were given to the 45 women in the intervention group during the first home visit conducted by an occupational therapist. This advice concerned modifications of the home environment, behavioural changes, and the use of assistive devices. Among the 45 women, 44 followed at least one of the guidelines, whereas one woman did not follow any. This woman experienced one fall during the observation period. When we excluded the woman who did not follow any advice from the analysis of the results, participants in the intervention group had a lower risk of experiencing one or more falls than controls: the unadjusted odds ratio was 0.271 (95% CI 0.082–0.899, p = 0.033). After adjustment for observation length, Barthel Index scores assessed before the beginning of the observation period, and body height, the odds ratio was 0.164 (95% CI 0.041–0.661, p = 0.011). Thirty-six of the 45 women in the intervention group followed at least half of the advice given during the first home visit conducted by an occupational therapist, whereas 9 women did not. Among these 9 poorly-adherent women, 4 experienced 5 falls. When we excluded the 9 women from the analysis of the results, participants in the intervention group had a lower risk of experiencing one or more falls than controls: the unadjusted odds ratio was 0.167 (95% CI 0.035–0.797, p = 0.025). After adjustment for observation length, Barthel Index scores assessed before the beginning of the observation period, and body height, the odds ratio was 0.104 (95% CI 0.018–0.612, p = 0.012).
Median Barthel Index score at the end of the study was 95, both in the patients belonging to the intervention group and in the controls (interquartile ranges were 85–100 and 90–100, respectively).
DISCUSSION
The absolute risk of experiencing one or more falls in our control group of home-dwelling women with a fall-related hip fracture was 26% (95% CI 13–39%), during a median observation time of 183 days after discharge from hospital. This risk appears to be lower than the 53% hazard reported by Shumway-Cook et al. (25) in a sample of 90 fallers with hip fracture, who lived in the community, at a 6-month follow-up after hospital discharge. We do not know the reasons underlying the discrepancy between our study and the previous one. It is possible that the multidisciplinary intervention we performed during in-patient rehabilitation effectively reduced fall risk, in agreement with the literature (2, 6). Recently, Kristensen et al. (26) reported a 32% proportion of fallers in a sample of 59 hip-fracture patients at a 6-month follow-up. An entry criterion of the last study was the ability to perform a Timed Up and Go test at a median of 10 days after surgery. As a consequence, the patients studied by Kristensen et al. (26) were strongly selected on the basis of their physical performance and are not easily comparable with our patients. In any case, the absolute risk of falling in our control group was relevant. We show that a single home visit by an occupational therapist conducted at a median of 20 days after discharge from hospital significantly reduced the proportion of fallers, after adjustment for length of observation, Barthel Index scores assessed before the beginning of the observation period, and body height. The occupational therapist suggested targeted modifications of home environment, behavioural changes, and use of assistive devices to prevent falls, after checking individual risk factors. The reduction in the risk of sustaining one or more falls attributable to the home visit was remarkable (the adjusted absolute risk fell from 26% to 8.8%). Furthermore, when we excluded from the analysis the women who did not follow any advice given during the home visit (n = 1) or those who did not follow at least 50% of the advice (n = 9), the adjusted absolute risk for sustaining falls dropped to 5.5% and 3.5%, respectively. The last results suggest that ameliorating the adherence to prevention advice may result in a further decrease in fall risk.
Several studies showed that home visits, mainly targeted at environmental hazards, significantly reduced the risk of falling in the elderly, but other reports did not (27–30). The originality of our study rests on the characteristics of the participants: to our knowledge, no previous reports have investigated the role of a home visit targeted at fall prevention in a sample of hip-fracture fallers following hospital discharge. Participant selection may represent a key factor in affecting the response to interventions for preventing falls, and may explain, at least in part, the discrepancies found in studies performed in non-homogeneous samples of elderly subjects (31) as well as the inconsistencies throughout different studies (27–30). The recommended approach for preventing falls in the elderly consists of a multidisciplinary programme based on the search for modifiable risk factors in individual subjects, followed by targeted interventions (2, 6, 8, 9). This approach has been used successfully in a sample of hip-fracture in-patients (19). Our subjects actually underwent a multidisciplinary intervention during in-patients rehabilitation. We show that a single home visit conducted after discharge from our hospital was effective in fall prevention, suggesting that an additive effect may be obtained by combining the 2 approaches (multidisciplinary intervention on in-patients and home visit following discharge from the hospital). Further studies are needed to test other types of home programmes targeted at fall prevention and their combination (2, 6, 32) to optimize the interventions in this group of subjects at high risk. Assessment of falls should be included in the evaluation of the outcome after rehabilitation in hip-fracture subjects (33, 34). Serum levels of 25-hydroxyvitamin D were very low in our sample, in agreement with various reports on elderly patients with hip fracture (35, 36). We did not show any significant associations between serum levels of 25-hydroxyvitamin D and fall risk. This result may be surprising, because several reports showed that vitamin D deficiency increases the risk of falling (20–22). However, our data may be explained by vitamin D supplementation, because we treated all the women with vitamin D (880 IU daily) after serum sample collection. Although the study was not powered to detect differences in the number of falls for each faller, there does not seem to be a difference with respect to the risk of a second fall between the 2 groups, because we found 20 falls in 13 fallers among the controls and 9 falls in 6 fallers in the intervention group. This result seems quite natural for the subgroup in which we failed to prevent the first fall.
Our study has several limitations. It evaluated a sample of home-dwelling white women living in a city, who sustained their first hip fracture due to a fall, were surgically operated on, were referred for in-patient rehabilitation, had no cognitive impairment, and returned home after discharge from the rehabilitation hospital. As a consequence, our results are not generalizable to the overall population of hip-fracture patients. Among the 119 women we randomized, 95 completed the study, whereas 24 did not. Of course, the aim was to retain a higher number of women after randomization. However, the specific features of our sample should be taken into account when considering the number of patients who did not complete the study. Sixteen of the 24 women who were lost did not return home at discharge from the rehabilitation hospital, because of acute concomitant diseases requiring a transfer to other hospitals or because of institutionalization at the end of in-patient rehabilitation. Both co-morbidities and institutionalization are very common conditions among hip-fracture survivors (12). The nature of the intervention prevented blinding of participants and complete blinding of hospital staff. The 2 occupational therapists who assessed falls were the same 2 who conducted all the home visits. This may have introduced a source of bias. However, falls were self-reported by the patients, and the occupational therapist simply recorded the self-reported falls. The follow-up period of the study was modest (about 6 months). However, the proportion of fallers among the controls was relevant (13 of 50, i.e. 26%), in spite of the relatively short period of observation. A longer period may be better to detect a greater number of fallers, but a greater proportion of patients lost to follow-up may be expected in these elderly, frail women. We did not record the time to the first fall: the occupational therapist, during both the first home visit in the intervention group and the home visit conducted in both groups at the end of the study, simply investigated the occurrence of falls and their number. Because no information was recorded on fall time, we were not able to perform a survival analysis of our data.
In conclusion, this study shows that a single home visit by an occupational therapist after discharge from a rehabilitation hospital significantly reduced the risk of falling in a sample of elderly women following their first hip fracture.
REFERENCES
1. Tinetti ME. Clinical practice: preventing falls in elderly persons. N Engl J Med 2003; 348: 42–49.
2. Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH. Intervention for preventing falls in elderly people. Cochrane Database Syst Rew 2003; CD000340.
3. Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med 2002; 18: 141–158.
4. Zijlistra GA, van Haastregt JC, van Rossum E, van Eijk JT, Yardley L, Kempen GI. Interventions to reduce fear of falling in community-living older people: a systematic review. J Am Geriatr Soc 2007; 55: 603–615.
5. Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med 1997; 337: 1279–1284.
6. Rubenstein LZ, Josephson KR. Falls and their prevention in elderly people: what does the evidence show? Med Clin North Am 2006; 90: 807–824.
7. Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J Am Geriatr Soc 2001; 49: 664–672.
8. Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA 2007; 297: 77–86.
9. Moylan KC, Binder EF. Falls in older adults: risk assessment, management and prevention. Am J Med 2007; 120: 493–496.
10. Saverino A, Benevolo E, Ottonello M, Zsirai E, Sessarego P. Falls in a rehabilitation setting: functional independence and fall risk. Eura Meddicophys 2006; 42: 179–184.
11. Parkkari J, Kannus P, Palvanen M, Natri A, Vainio J, Aho H, et al. Majority of hip fractures occur as a result of a fall and impact on the greater trochanter of the femur: a prospective controlled hip fracture study with 206 consecutive patients. Calcif Tissue Int 1999; 65: 183–187.
12. Physician’s guide to prevention and treatment of osteoporosis. Washington DC: The National Osteoporosis Foundation; 2003.
13. Colon-Emeric C, Kuchibhatla M, Pieper C, Hawkes W, Fredman L, Magaziner J, et al. The contribution of hip fracture to risk of subsequent fractures: data from two longitudinal studies. Osteoporos Int 2003; 14: 565–574.
14. Di Monaco M, Di Monaco R, Manca M, Cavanna A. Functional recovery and length of stay after recurrent hip fracture. Am J Phys Med Rehabil 2002; 81: 86–89.
15. Rodaro E, Pasqualini M, Iona LG, Di Benedetto P. Functional recovery following a second hip fracture. Eura Medicophys 2004; 40: 179–183.
16. Stenvall M, Elinge E, von Heideken Wagert P, Lundstrom M, Gustafson Y, Nyberg L. Having had a hip fracture: association with dependency among the oldest old. Age Ageing 2005; 34: 294–297.
17. Siris ES. Patients with hip fracture: what can be improved? Bone 2006; 38: S8–S12.
18. Hauer K, Rost B, Rutschle K, Opitz K, Specht N, Bartsch P, et al. Exercise training for rehabilitation and secondary prevention of falls in geriatric patients with a history of injurious falls. J Am Geriatr Soc 2001; 49: 10–20.
19. Stenvall M, Olofsson B, Lundstrom M, Englund U, Borssen B, Svensson O, et al. A multidisciplinary, multifactorial intervention program reduces postoperative falls and injuries after femoral neck fracture. Osteoporos Int 2007; 18: 167–175.
20. Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, Staehelin HB, Bazemore MG, Zee RY, Wong JB. Effect of Vitamin D on falls: a meta-analysis. JAMA 2004; 291: 1999–2006.
21. Jackson C, Gaugris S, Sen SS, Hosking D. The effect of cholecalciferol (vitamin D3) on the risk of fall and fracture: a meta-analysis. QJM 2007; 100: 185–192.
22. Bischoff-Ferrari HA. How to select the doses of vitamin D in the management of osteoporosis. Osteoporos Int 2007; 18: 401–407.
23. Haines TP, Bennell KL, Osborne RH, Hill KD. Effectiveness of targeted falls prevention programme in subacute hospital setting: randomised controlled trial. BMJ 2004; 328: 676–683.
24. Mahoney F, Barthel D. Functional evaluation: the Barthel index. Md State Med J 1965; 14: 61–65.
25. Shumway-Cook A, Ciol MA, Gruber W, Robinson C. Incidence of and risk factors for falls following hip fracture in community-dwelling older adults. Phys Ther 2005; 85: 648–655.
26. Kristensen MT, Foss NB, Kehlet H. Timed “up & go” test as a predictor of falls within 6 month after hip fracture surgery. Phys Ther 2007; 87: 24–30.
27. van Haastregt JC, Diederiks JP, van Rossum E, de Witte LP, Crebolder HF. Effects of preventive home visits to elderly people living in the community: systematic review. BMJ 2000; 320: 754–758.
28. Pardessus V, Puisieux F, Di Pompeo C, Gaudefroy C, Thevenon A, Dewailly P. Benefits of home visits for falls and autonomy in the elderly: a randomized trial study. Am J Phys Med Rehabil 2002; 81: 247–252.
29. Cumming RG, Thomas M, Szonyi G, Salkeld G, O’Neill E, Westbury C, Frampton G. Home visits by an occupational therapist for assessment and modification of environmental hazards: a randomized trial of falls prevention. J Am Geriatr Soc 1999; 47: 1397–1402.
30. Nikolaus T, Bach M. Preventing falls in community-dwelling frail older people using a home intervention team (HIT): results from the randomized Falls-HIT trial. J Am Geriatr Soc 2003; 51: 300–305.
31. Lord SR, Tiedemann A, Chapman K, Munro B, Murray SM, Sherrington C. The effect of an individualized fall prevention program on fall risk and falls in older people: a randomized, controlled trial. J Am Geriatr Soc 2005; 53: 1296–1304.
32. Inokuchi S, Matsusaka N, Hayashi T, Shindo H. Feasibility and effectiveness of a nurse-led community exercise programme for prevention of falls among frail elderly people: a multicentre controlled trial. J Rehabil Med 2007; 39: 479–485.
33. Di Monaco M, Vallero F, Di Monaco R, Mautino F, Cavanna A. Functional recovery after concomitant fractures of both hip and upper limb in elderly people. J Rehabil Med 2003; 35: 195–197.
34. Stenvall M, Olofsson B, Nyberg L, Lundstrom M, Gustafson Y. Improved performance in activities of daily living and mobility after a multidisciplinary postoperative rehabilitation in older people with femoral neck fracture: a randomized controlled trial with 1-year follow-up. J Rehabil Med 2007; 39: 232–238.
35. Di Monaco M, Vallero F, Di Monaco R, Mautino F, Cavanna A. Serum levels of 25-hydroxyvitamin D and functional recovery after hip fracture. Arch Phys Med Rehabil 2005; 86: 64–68.
36. Di Monaco M, Vallero F, Di Monaco R, Tappero R, Cavanna A. 25-hydroxyvitamin D, parathyroid hormone, and functional recovery after hip fracture in elderly patients. J Bone Miner Metab 2006; 24: 42–47.