OBJECTIVE: To explore the influence of workers’ compensation coverage on injury patterns and return-to-work outcome in orthopaedic injuries of the extremities.
DESIGN: Prospective and follow-up study.
SUBJECTS: A total of 154 subjects were recruited and 37.7% of the injuries were covered by workers’ compensation.
METHODS: Baseline data were obtained by questionnaire and chart review. The main outcome variable was time of first return to work. Subjects were followed up at 1, 3 and 6 months after initial interview. Cox proportional hazards model was used to analyse associations between potential predictors and return-to-work.
RESULTS: The workers’ compensation group were most likely to be men employed in labour occupations and were most likely to sustain crushing injuries, or injuries from being struck by objects. The 6-month return-to-work rates for the workers’ compensation and non-workers’ compensation groups were 70.7% and 71.9%. Early return-to-work was associated with more years in higher education, and increased self-efficacy in both groups. Moreover, age older than 45 years and hospitalization less than 14 days were associated with early return-to-work in the non-workers’ compensation group.
CONCLUSION: The injury patterns of workers’ compensation and non-workers’ compensation groups differed, but the likelihood of return-to-work at 6-month follow-up was similar. More years of education and self-efficacy were positive predictors of return-to-work.
Key words: return to work, occupational injuries, workers’ compensation.
J Rehabil Med 2008; 40: 440–445
Correspondence address: Huey-Wen Liang, Department of Physical Medicine and Rehabilitation, National Taiwan University Hospital, 7 Chong-Shan S. Road, 100 Taipei, Taiwan. E-mail: lianghw@ntu.edu.tw
Submitted September 9, 2007; accepted January 29, 2008
Introduction
Traumatic limb injury is a leading cause of work disability (1). Studies of motor vehicle accidents and occupational injuries revealed that upper and lower extremities are the most commonly injured sites (2–4). The number of lost working days and lost productivity associated with these injuries are high (2). However, survivors of severe injuries can achieve a quality of life comparable with the normal population after returning to their former jobs (5). Therefore, the goals of rehabilitating injured patients should be functional independence and return-to-work (RTW).
In order to maximize the proportion of workers returning to work, the negative predictors that may hamper the outcome should be identified. Previous studies have documented the complex function of bio-psycho-social factors associated with RTW outcome in cases of traumatic injuries, occupational injuries and back pain (3, 6, 7). Among the various associated factors, financial compensation has been linked with delayed RTW in workers who had sustained lower back pain, neck pain and neck injuries (8–12). Provision of payments for pain and suffering, in addition to medical and income-replacement benefits, has been revealed to delay the closure of claims following whiplash injuries (11). The causal relationship between compensation and outcome was not well understood, but the theory that compensation is a potential barrier to delay recovery might impose unfavourable opinion to the cases covered by compensation. The extent to which workers’ compensation negatively influences injury outcome is uncertain. Moreover, any potential confounding factor in the causal relationship between compensation and RTW should be investigated carefully. Increased risk of occupational injuries has been reported according to gender or type of occupation (13). Injuries treated on an emergent case basis tended to be of different aetiologies, depending on whether they occurred in the workplace (14). These findings indicate that the injury patterns and personal characteristics of individuals depend on whether they are covered by workers’ compensation (WC). However, whether any bias is involved in the relationship between RTW and WC requires further exploration.
The WC system in Taiwan is a compulsory national programme, and has insured 7.8–8.6 million workers in the past 5 years (15). This system provides no-fault compensation for all medical expenses and temporary and partial income replacement if workers are unable to earn wages because of their occupational injuries. The system provides income replacement for 70% of salary during the first year and 50% during the second year. Inability to RTW requires certification by a physician. Injuries sustained while commuting to and from work are viewed as occupational injuries only if no traffic regulations were violated. If the injuries are not occupation-related and require 4 or more days of hospitalization, then the insured worker can qualify for sickness benefits at the rate of 50% of insured salary.
In this study, we hypothesized that WC affects injury patterns and outcomes. The investigation describes the demographic and occupational characteristics of patients hospitalized for orthopaedic trauma, according to whether they were receiving workers’ compensation. The incidence and determinants of RTW after injuries are also examined by comparing these 2 groups of subjects. The study helps to clarify whether RTW is associated with receipt of WC benefits.
Material and Methods
Patients
Patients diagnosed with upper and/or lower limb injuries and hospitalized in the orthopaedic and plastic surgery wards in 2 university hospitals were enrolled into the study. Inclusion criteria were: 18–65 years of age, full-time employed before injury, and hospitalization within 14 days of injury. The following subjects were excluded: those unable to read or answer the questionnaires, foreign workers, and those with coexisting injuries to the central nervous system (i.e. traumatic brain injuries or spinal cord injury) or internal organs. No subjects had required resuscitation or suffered shock. Consecutive cases were collected from July 2004 to December 2005 in selected wards. Thus, 209 subjects met the study criteria, and 165 (78.9%) subjects answered the questionnaires. A total of 154 subjects with complete data were analysed. The mean age was 36.9 years (standard deviation (SD) 10.9) and 75% of the subjects were men. The study was approved by the ethics committee at each participating hospital and informed consent was obtained from all participants.
Methods
All eligible subjects answered the baseline questionnaires regarding personal data (age, gender, marital status, education level, smoking and alcoholic consumption) and occupational history (job titles and seniority). Occupations were categorized into 4 groups. Group 1 included manager and professionals and group 2 included technical, sales, administration and service personnel. These 2 groups were classified as white-collar workers. Workers in farming, forestry and fishing industries were classified as group 3 and group 4 included repairs, machine operators and labourers. Group 3 and 4 were categorized as blue-collar workers.
Each patient’s injury history was obtained from the questionnaire. The medical charts were reviewed for the following information: diagnosis, date of admission and discharge, causes or mechanisms of injuries, injury date, whether or not the injury was work-related and surgical treatment for injury. Injury mechanisms were classified as high-energy (traffic accident, fall from height or struck by falling object) or low-energy (cutting, crashing, or crushing). Additionally, the injuries were grouped according to presence of fracture and involvement of upper or lower limbs. The injuries insured by WC were classified as the WC group and the others were classified as the non-WC group. The information was collected by patient interview. Job satisfaction was rated on a 5-point Likert scale. One question adapted to measure the self-efficacy of RTW was, “What is the likelihood of your returning to work within one month?”. The respondents scored their estimates from 1 (no chance) to 5 (very high).
All subjects were followed up after 1, 3 and 6 months by telephone, post, or interview at out-patient clinics. The follow-up questionnaire included RTW status and the date the subject first returned to work, if applicable.
Statistics
Descriptive statistics were presented as means, SD and percentages, as applicable. The 2 groups were compared by χ2 for categorical variables and t-test for continuous variables. Life table and Kaplan-Meier estimate analysis was applied to compute and plot cumulative proportions of RTW and a Cox proportional hazards regression model was used to examine the effect of personal, occupational and injury factors on the primary outcome, the time (in days) between injuries to the date of RTW for both groups. The independent variables were personal factors (age, gender, marital status and educational level), occupational factors (occupations and job seniority), injury factors (injury types, injury sites and hospitalization days) and psychosocial factors (job satisfaction and self-efficacy). The final model was determined by stepwise selection. The SPSS software (Version 13.0, SPSS Inc. Chicago, IL, USA) was used for all statistical analysis.
Results
Demographic data
Of the injuries 38.7% were classified as WC group, which was similar in age, years of education and marital status to the non-WC group (Table I). Nevertheless, the WC group had a higher proportion of men (86.2% vs 67.7%) and production workers/repair workers/operators/labourers. Additionally, a significant difference between white-collar and blue-collar workers was observed. Blue-collar workers tended to have higher proportion of men (38.3% vs 11.0 %), educational years less than 9 years (39.7% vs 18.5%) and people receiving WC (47.9% vs 28.4%).
| Table I. Demographic data of the 154 subjects |
| Variables | Total (n = 154) | Non-workers’ compensation group (n = 96) | Workers’ compensation group (n = 58) | p |
| Age (years), mean (SD) | 36.9 (10.9) | 36.4 (11.3) | 37.8 (10.1) | 0.43 |
| Men, n (%) | 115 (74.7) | 65 (67.7) | 50 (86.2) | 0.01 |
| Marital status, n (%) | | | | 0.48 |
| Married | 84 (54.5) | 50 (52.1) | 34 (58.6) | |
| Single | 64 (41.6) | 41 (42.7) | 23 (39.7) | |
| Other | 6 (3.9) | 5 (5.2) | 1 (1.7) | |
| Years of education, n (%) | | | | 0.52 |
| ≤ 9 | 44 (28.6) | 30 (31.3) | 14 (24.1) | |
| > 9–12 | 66 (42.9) | 38 (39.6) | 28 (48.3) | |
| > 12 | 44 (28.6) | 28 (29.2) | 16 (27.6) | |
| Holding other insurance for accidents, n (%) | 70 (45.8) | 43 (44.8) | 27 (47.4) | 0.76 |
| Occupation, n (%) | | | | 0.02 |
| Manager/professional | 20 (13.0) | 11 (11.5) | 9 (15.5) | |
| Technical/sales/administration/service | 61 (39.6) | 47 (49.0) | 14 (24.1) | |
| Farming/forestry/fishing | 6 (3.9) | 4 (4.2) | 2 (3.4) | |
| Production/repairs/operators/labourers | 67 (43.5) | 34 (35.4) | 33 (56.9) | |
| SD: standard deviation. |
Injury conditions
Traffic accident accounted for half of all causes of injuries and up to 60% in the non-WC group (Table II). Conversely, the WC group was more likely to have sustained crashing or crushing injuries. Most were admitted shortly after injury (median: 0 days between injuries to admission) and most had undergone operation (96.8%). The overall average days of hospitalization was 11.0 (median: 8 days) and did not significantly differ between the 2 groups. The self-efficacy of returning to work within one month was mostly low, with only 23.5% indicating the probability was “high” or “very high” (Table II).
| Table II. Injury characteristics and medical history of the 154 subjects |
| Variables | Total (n = 154) n (%) | Non-workers’ compensation group (n = 96) n (%) | Workers’ compensation group (n = 58) n (%) | p |
| Cause of injuries | | | | < 0.001 |
| Traffic accident | 78 (50.6) | 57 (59.4) | 21 (36.2) | |
| Crashing injury | 17 (11.0) | 5 (5.2) | 12 (20.7) | |
| Crushing injury | 17 (11.0) | 4 (4.2) | 13 (22.4) | |
| Penetrating injury | 8 (5.2) | 6 (6.3) | 2 (3.4) | |
| Fall from height | 11 (7.1) | 6 (6.3) | 5 (8.6) | |
| Level fall | 17 (11.0) | 14 (14.6) | 3 (5.2) | |
| Others | 6 (3.9) | 4 (4.2) | 2 (3.4) | |
| High-energy injuries | 91 (59.5) | 62 (65.3) | 29(50.0) | 0.06 |
| Injury sites | | | | 0.30 |
| Major joint or long bone fracture of lower limbs | 54 (35.1) | 37 (38.5) | 17 (29.3) | |
| Foot fracture or soft tissue injury of lower limbs | 14 (9.1) | 6 (6.3) | 8 (13.8) | |
| Major joint or long bone fracture of upper limbs | 38 (24.7) | 25 (26.0) | 13 (22.4) | |
| Hand fracture or soft tissue injury of upper limbs | 37 (24.0) | 20 (20.8) | 17 (29.3) | |
| Multiple injuries | 11 (7.1) | 8 (8.3) | 3 (5.2) | |
| Self-confidence of return to work in one month | | | | 0.39 |
| No chance | 86 (57.7) | 52 (56.5) | 34 (59.6) | |
| Low chance | 20 (13.4) | 13 (14.1) | 7 (14.3) | |
| Moderate chance | 8 (5.4) | 5 (5.4) | 3 (5.3) | |
| High chance | 14 (9.4) | 6 (6.5) | 8 (14.0) | |
| Very high chance | 21 (14.1) | 16 (17.4) | 5 (8.8) | |
| Days between injury and admission, mean (SD) | 0.8 (2.7) | 0.8 (2.6) | 0.8 (2.9) | 0.19* |
| Receiving operation | 149 (96.8) | 92 (95.8) | 57 (98.3) | 0.65 |
| Days of hospitalization, mean (SD) | 11.0 (10.9) | 11.0 (11.4) | 11.1 (10.1) | 0.95* |
| *Mann-Whitney U test. SD: standard deviation. |
Follow-up conditions
The 6-month follow-up rate was 83.8% and was similar in the WC and non-WC groups (Table III). The 25 cases lost to follow-up had a higher proportion of multiple injuries (upper and lower extremity) and of fewer educational years than the followed cases, but the age, hospitalization and job tenure was similar between them. Of the follow-up cases, 110 of 129 (85.3%) returned to work within 6 months of injury. Among those RTW, 86 (78.2%) subjects returned to the same job and the same worksite. Receiving medical treatment or undergoing rehabilitation was the major reason reported for not returning to work during 3 follow-up occasions.
| Table III. Follow-up data of the154 subjects |
| | Total (n = 154) | Non-workers’ compensation group (n = 96) | Workers’ compensation group (n = 58) |
| Mean follow-up days, mean (SD) | 83.1 (60.5) | 78.4 (59.8) | 90.9 (61.5) |
| Lost follow-up, n (%) | 25 (16.2) | 15 (15.6) | 10 (17.2) |
| Return to work at 6 months, n (%) | 110 (71.4) | 69 (71.9) | 41 (70.7) |
| To the same job, the same worksite | 86 (55.8) | 53 (55.2) | 33 (56.9) |
| To different job, the same worksite | 15 (9.7) | 10 (10.4) | 5 (8.6) |
| To different worksite | 9 (5.8) | 6 (6.3) | 3 (5.2) |
Determinants of early return-to-work
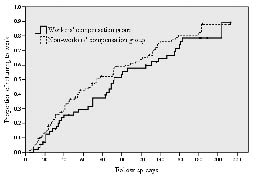
The cumulative proportions of returning to work were similar between WC and non-WC groups (Fig. 1). The median time for both groups was 92.3 and 74.2 days, respectively (p = 0.20 by life table analysis). Nevertheless, Cox proportional hazard modelling showed different predictors in these 2 groups. Higher self-efficacy and more years of education were associated early RTW in both groups (Table IV). The non-WC cases who had received low-energy injuries or who were hospitalized for 14 days or less returned to work earlier than those who had received high-energy injuries or who were hospitalized for more than 14 days. Furthermore, subjects over 44 years of age were more likely to return to work early than those younger than 25 years (adjusted relative rate ratio: 2.57; 95% confidence interval: 1.12–5.87).
Fig. 1. Accumulated proportion returning to work after injuries, using Kaplan-Meier analysis, grouped by whether or not subjects were receiving workers’ compensation.
| Table IV. Relative odds ratio (OR) and 95% confidence intervals (95% CI) of returning to work (RTW) after injuries by proportional hazards regression analysis |
| Variable | Non-workers’ compensation group | Workers’ compensation group |
| Unadjusted relative OR (CI 95%) | Adjusted relative OR (CI 95%) | Unadjusted relative OR (CI 95%) | Adjusted relative OR (CI 95%) |
| Women | 1.03 (0.62, 1.72) | 1.69 (0.96, 2.97) | 1.05 (0.41, 2.68) | 2.31 (0.6, 7.75) |
| Age (years) | | | | |
| < 25 | Reference | Reference | Reference | Reference |
| 25–44 | 1.29 (0.69, 2.40) | 1.39 (0.48, 2.36) | 0.79 (0.26, 2.42) | 0.50 (0.14, 1.80) |
| > 44 | 1.35 (0.67, 2.70) | 2.39 (1.05, 5.47) | 0.41 (0.12, 1.35) | 0.31 (0.61, 1.53) |
| Years of education | | | | |
| ≤ 9 | Reference | Reference | Reference | Reference |
| >9–12 (1) | 1.71 (0.93, 3.15) | 1.41 (0.66, 3.02) | 3.11 (1.17, 8.26) | 3.97 (1.20, 13.15) |
| > 12 (2) | 2.17 (1.14, 4.13) | 2.09 (1.07, 5.67) | 3.70 (1.27, 10.78) | 4.78 (1.32, 17.26) |
| Self-efficacy of RTW |
| None | Reference | Reference | Reference | Reference |
| A little | 1.88 (0.92, 3.83) | 2.71 (1.23, 5.98) | 1.72 (0.64, 4.62) | 2.30 (0.69, 7.60) |
| Moderate | 1.14 (0.40, 3.20) | 0.86 (0.29, 2.59) | 1.13 (0.26, 4.85) | 1.55 (0.32, 7.53) |
| High | 2.00 (0.71, 5.68) | 2.23 (0.74, 6.70) | 3.45 (1.47, 8.09) | 2.87 (1.11, 13.15) |
| Very high | 5.15 (2.67, 9.91) | 4.88 (2.31, 10.31) | 5.20 (1.38, 19.54) | 11.14 (2.40, 51.59) |
| Injury of low-energy | 2.37 (1.45, 3.88) | 2.48 (1.37, 4.50) | – | – |
| Hospitalization ≤ 14 days | 3.13 (1.26, 7.81) | 3.39 (1.17, 9.79) | – | – |
Discussion
This prospective study demonstrates that 85.3% of followed cases could return to work 6 months after hospitalization for orthopaedic injuries. Subject characteristics and determinants of early RTW differed according to whether subjects were insured by WC. Such discrimination has rarely been highlighted in previous studies and the clinical significance should be further examined.
A higher proportion of crashing or crushing injuries were observed among the WC group, and these findings were consistent with an earlier UK study that examined only male subjects (14). Furthermore, the WC group also included a higher proportion of men and blue-collar workers. By contrast, the UK study indicated that work-related injuries tended to involve older workers, be low in severity, and be more likely to cause litigation and symptoms of post-traumatic stress disorders (14). Our study also found that injured workers insured by WC had different demographic and occupational features from uninsured workers. As reported elsewhere, manufacturing or agricultural workers had a higher risk of upper limb amputation or fracture (16). In addition, analytical results demonstrate that blue-collar tended to be male, less educated and likely to be under WC. Higher physical demands of jobs and disadvantageous socioeconomic status of this population was likely to influence RTW outcome.
During the 6-month period of this study, an 85% RTW rate was observed, which was consistent with previously reported results. However, we could not rule out the possibility of overestimating the RTW, because the 25 cases lost to follow-up had a higher proportion of multiple injuries and fewer years of education than the followed cases. A wide range of clinical conditions were investigated herein, but almost all were fracture and soft tissue injuries of the upper and lower limbs. The injury severity of our subjects was comparatively lower than that in studies which enrolled cases at territory trauma centres, but higher than that of unhospitalized cases (17, 18). McKenzie et al. (18) demonstrated that the cumulative proportion of subjects returning to work at 3, 6, 12, 24 and 84 months was 12%, 28%, 42%, 51% and 58%, respectively. Conversely, the average sick leave from work was only 3 weeks in outpatients with fractures of wrist, hand or foot bones (19).
The predictors of RTW identified in the present report, i.e. education level, self-efficacy and injury types, were consistent with previous studies (6, 18, 20, 21). Other previously documented factors, such as gender, job tenure, alcohol consumption, occupation, workers’ compensation claims, and job satisfaction, did not demonstrate any association with RTW at follow-up. This study did not support prior findings that compensation was a negative predictor of RTW. One possible explanation is that the wage replacement (70% of insured wages) was probably inadequate for most labourers, since workers in Taiwan often insure themselves at lower wages in order to reduce premiums. The average insured monthly wages for 2005 was NT$26,145 (approximately US$800), but the average income for the same year was US$1170 (15). Furthermore, the different demographic and occupational features in the WC and non-WC group may also confound the effect of WC on RTW.
Because the WC cases had several different features from the non-WC group, the groups were analysed separately. These 2 groups were similar in factors associated with early RTW, with the exception of age, injury types (high- or low-energy) and hospitalization days. The injury types and hospitalization days were regarded as proxies of injury severity, which is considered an important outcome predictor in injured patients (6, 20, 22). The absence of association with RTW in the WC group was probably due to the smaller sample size. Previous research has produced inconsistent results regarding age. MacKenzie et al. (17) reported that a younger population had a greater likelihood of RTW following severe trauma of the lower limbs, but Pransky et al. (3) reported the opposite findings. An older population (over 40 years of age) tended to have a favourable outcome in the non-WC group, not in the WC group. A possible explanation is that the shorter tenure and lower job experience made returning to work problematic in the younger group without WC coverage.
This study had the following limitations: The injury profiles and psychosocial factors may not have been sufficiently comprehensive, despite efforts to include major risk factors. For example, a 5-point Likert scale was adapted to measure job satisfaction and self-efficacy. Secondly, the cases were managed by different physicians and methods, which might have influenced the outcome (23, 24). Because more than 95% of the subjects had undergone surgery and no evidence was found that WC would influence the practice of the treating physicians, bias was regarded as unlikely or insignificant. Thirdly, the results could not be generalized beyond the follow-up period. Furthermore, first RTW was examined, which indicated the end of only one of possibly several episodes of work disability caused by the original injury (25). Finally, only 73% of the eligible cases participated in the study, which might limit the representativeness of the results.
In conclusion, patients hospitalized with orthopaedic injuries show different injury patterns in terms of WC claims, which should be taken into account when investigating the outcome of occupational injuries. The WC group in this study had a higher proportion of males and blue-collar workers than the non-WC group, and also sustained more crashing and crushing injuries. WC coverage was not associated with RTW outcome. Both higher education and higher self-efficacy were positively linked with likelihood of RTW, regardless of whether the subject was receiving WC.
Acknowledgements
The authors would like to thank the Bureau of Health Promotion, Department of Health, Taiwan of the Republic of China, Taiwan for financially supporting this research under Contract No. DOH94-HP-1405.
References
1. Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ. Selected major risk factors and global and regional burden of disease. Lancet 2002; 360: 1347–1360.
2. Ebel BE, Mack C, Diehr P, Rivara FP. Lost working days, productivity, and restraint use among occupants of motor vehicles that crashed in the United States. Inj Prev 2004; 10: 314–319.
3. Pransky GS, Benjamin KL, Savageau JA, Currivan D, Fletcher K. Outcomes in work-related injuries: a comparison of older and younger workers. Am J Ind Med 2005; 47: 104–112.
4. Liu YH, Lin MR, Wang JD. Cost and determinants of morbidity from work related disabling injuries in Taiwan. Occup Environ Med 199; 52: 138–142.
5. Post RB, Sluis VD, Duis HJT. Return to work and quality of life in severely injured patients. Disabil Rehabil 2006; 28: 1399–1404.
6. MacKenzie EJ, Shapiro S, Smith RT, Siegel JH, Moody M, Pitt A. Factors influencing return to work following hospitalization for traumatic injury. Am J Public Health 1987; 39: 625–631.
7. Schultz IZ, Crook J, Meloche GR, Berkowitz J, Milner R, Zuberbier OA, et al. Psychosocial factors predictive of occupational low back disability: towards development of a return-to-work model. Pain 2004; 107: 77–85.
8. Lysgaard AP, Fonager K, Nielsen CV. Effect of financial compensation on vocational rehabilitation. J Rehabil Med 2005; 37: 388–391.
9. McNaughton HK, Sims A, Taylor WJ. Prognosis for people with back pain under a no-fault 24-hour-cover compensation scheme. Spine 2000 15; 25: 1254–1258.
10. Rasmussen C, Rechter L, Schmidt I, Hansen VK, Therkelsen K. The association of the involvement of financial compensation with the outcome of cervicobrachial pain that is treated conservatively. Rheumatol 2001; 40: 552–554.
11. Cassidy JD, Carroll LJ, Côté P, Lemstra M, Berglund A, Nygren Å. Effect of eliminating compensation for pain and suffering on the outcome of insurance claims for whiplash injury. N Engl J Med 2007; 342: 1179–1186.
12. Scuderi GJ, Sherman AL, Brusovanik GV, Pahl MA, Vaccaro AR. Symptomatic cervical disc herniation following a motor vehicle collision: return to work comparative study of workers’ compensation versus personal injury insurance status. Spinal J 2005; 5: 639–644.
13. Islam SS, Velilla AM, Doyle EJ, Ducatman AM. Gender differences in work-related injury/illness: analysis of workers compensation claims. Am J Ind Med 2001; 39: 84–91.
14. Mason S, Wardrope J, Turpin G, Rowlands A. Outcomes after injury: a comparison of workplace and nonworkplace injury. J Trauma 2002; 53: 98–103.
15. Taiwan Bureau of Labor Insurance. Statistics of labor insurance in Taiwan 2005. Taipei: Taiwan Bureau of Labor Insurance; 2006.
16. Islam SS, Biswas RS, Nambiar AM, Syamlal G, Velilla AM, Ducatman AM, et al. Incidence and risk of work-related fracture injuries: experience of a state-managed workers’ compensation system. J Occup Environ Med 2001; 43: 140–146.
17. MacKenzie EJ, Morris JA, Jr., Jurkovich GJ, Yasui Y, Cushing BM, Burgess AR, et al. Return to work following injury: the role of economic, social, and job-related factors. Am J Public Health 1998; 88: 1630–1637.
18. MacKenzie EJ, Bosse MJ, Kellam JF, Pollak AN, Webb LX, Swiontkowski MF, et al. Early predictors of long-term work disability after major limb trauma. J Trauma 2006; 61: 688–694.
19. Lee RH. Length of sickness absence from work after minor fractures. Int J Rehabil Res 1982; 5: 499–506.
20. Tate DG. Workers’ disability and return to work. Am J Phys Med Rehabil 1992; 71: 92–96.
21. Seland K, Cherry N, Beach J. A study of factors influencing return to work after wrist or ankle fractures. Am J Ind Med 2006; 49: 197–203.
22. Meerding WJ, Looman CW, Essink-Bot ML, Toet H, Mulder S, van Beeck EF. Distribution and determinants of health and work status in a comprehensive population of injury patients. J Trauma 2004; 56: 150–161.
23. Tufescu TV, Buckley R. Age, gender, work capability, and worker’s compensation in patients with displaced intraarticular calcaneal fractures. J Orthop Trauma 2001; 15: 275–279.
24. Stevens DG, Beharry R, McKee MD, Waddell JP, Schemitsch EH. The long-term functional outcome of operatively treated tibial plateau fractures. J Orthop Trauma 2001; 15: 312–320.
25. Baldwin ML, Johnson WG, Butler RJ. The error of using returns-to-work to measure the outcomes of health care. Am J Ind Med 1996; 29: 632–641.