OBJECTIVE: The aim of this study was to compare muscle activation patterns and patellofemoral joint morphologies between patients with knee osteoarthritis with and without patellar malalignment.
SUBJECTS: The subjects were divided into 3 groups. Group A comprised 11 patients with symptomatic knee osteoarthritis without patellar malalignment. Group B comprised 14 patients with symptomatic knee osteoarthritis with patellar malalignment. Group C comprised 10 age-matched subjects with non-knee osteoarthritis as controls.
METHODS: Isokinetic dynamometry with surface electromyography was used to measure maximal muscle activity in terms of vastus medialis oblique/vastus lateralis ratios. Merchant’s view was taken to analyse the bony anatomy of the patellofemoral joint. Recordings were made at angular velocities of 80, 120 and 240º/sec.
RESULTS: The electromyographic ratios of group B were lower than groups A and C for all testing velocities (p < 0.05). Group B also had larger sulcus angles, lateral patellar tilt and displacement. The electromyographic ratios correlated negatively with sulcus angles.
CONCLUSION: Subjects with knee osteoarthritis with patellar malalignment exhibited an imbalance in quadriceps contraction, as confirmed by altered vastus medialis oblique/vastus lateralis ratios associated with larger sulcus angles of the patellofemoral joints. The sulcus angle may be an important contributing factor in causing abnormal patellar tracking in knee osteoarthritis.
Key words: osteoarthritic knee, patellar malalignment, electromyography, vastus medialis oblique, vastus lateralis, bony structure, sulcus angle.
J Rehabil Med 2008; 40: 381–386
Correspondence address: Simon F.T. Tang, Department of Physical Medicine and Rehabilitation, Chang Gung Memorial Hospital, No 5, Fu-Hsin Street, Kuei Shan, Tao-Yuan, 333, Taiwan. E-mail: fttang@adm.cgmh.org.tw
Submitted February 5, 2007; accepted January 2, 2008
Introduction
Patellar malalignment is a common aspect of osteoarthritic knee that is observed regularly in clinics, either in isolation or in conjunction with tibiofemoral (TF) joint osteoarthritis (OA) (1–3). The clinical features of patellar malalignment are similar to those of other patellofemoral pain syndromes (PFPS). Patellar malalignment is a translational or rotational deviation of the patella relative to any axis, such as subluxation or tilting (4). Lateral subluxation is frequently accompanied by tilt. The combination of subluxation and tilting usually leads to arthrosis due to abnormal loading of the articular cartilage (5). Recent studies on patellar arthrosis have demonstrated that several factors may increase the risk of patellar arthrosis, including patellofemoral joint (PFJ) anatomy, limb alignment, soft tissue stabilizers and muscular activation pattern (6). Several studies have suggested that the lack of equilibrium between the vastus medialis oblique (VMO) and the vastus lateralis (VL) is a risk factor resulting in abnormal patellar tracking (7–9). An in vitro study by Sakai et al. (7) indicated that weakness of the VMO could cause lateral shift of the patella at 0° and 15° of knee flexion. Souaz et al. (8) compared the VMO/VL electromyographic (EMG) ratios of healthy subjects and patients with PFPS, and found that the patients’ ratios were lower than those of healthy subjects during concentric contraction exercises, which might suggest the existence of a weakness in the VMO. Similar findings were shown in a study by Tang et al. (9). Moreover, based on patellar morphology, some authors suggest that a decreased depth of the trochlear groove might be a primary cause of abnormal patellar movement (10, 11). Farrhmand et al. (10) suggested that the slope of the lateral facet of the groove remained the primary determinant of resistance to lateral patellar subluxation. Through the revision of various studies of patellar arthrosis, the muscle imbalance between the VMO and the VL and the bony structure of the knee are both likely to contribute to the development of PFPS. However, whether muscular imbalance and the bony anatomy of the PFJ are precursors to, or the result of, knee OA with patellar malalignment is an interesting question. One hypothesis is that the medial TF osteoarthritic knee may develop early due to mechanical factors such as obesity and meniscectomy or quadriceps weakness. PFJ involvement may occur later due to the development of local factors such as a patellar tracking abnormality, which are secondary to the malalignment resulting from progressive medial TF OA (12, 13). However, these hypotheses about the progression that will lead to combined pattern of knee OA with patellar malalignment are still presumptive and require evidence based on a prospective methodology.
Understanding the effect of abnormal patellar tracking on the process of OA might have important implications for the rehabilitation of patients with osteoarthritic knee. The aim of this study was therefore to compare the bony anatomy of the PFJ by radiograph of Merchant’s view in order to investigate the relationship between surface VMO/VL EMG ratio and PFJ morphology in osteoarthritic knee patients with and without patellar malalignment. Since angular velocity with an isokinetic dynamometer is important in muscle performance, we also examined the effect of angular velocity on EMG ratio during dynamic knee extension. In this study, our first hypothesis was that the VMO/VL ratio would be lower in patients with osteoarthritic knee with patellar malalignment, and the second that there would be a significant correlation between the anatomical data and EMG ratio in patients with osteoarthritic knee with and without patellar malalignment.
Material and methods
Subjects
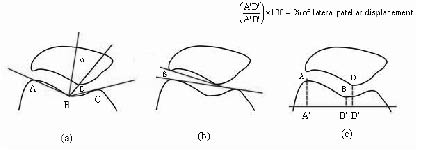
Twenty-five subjects with symptomatic osteoarthritic knee were included in this study and separated into 2 groups (experimental groups), one group comprised 11 patients with TF OA with normal patellar alignment (group A) and the other comprised 14 patients with TF OA with patellar malalignment (group B) (Fig. 1). Ten age-matched healthy subjects were recruited and served as controls (group C). The severity of the osteoarthritic knee was diagnosed as stage I or II according to the Ahlbäck’s grading by anteroposterior radiography (14). Knees with or without patellar malalignment were diagnosed by Merchant’s view, which was obtained in the supine position with the knee flexed at 45° (15). All subjects signed an informed consent form before participating. Pain symptoms and the activities of daily living of the patients with osteoarthritic knee were assessed using the Lequesne’s Index (16). The 2 OA groups had similarly score in Lequesne’s Index with moderate severity. The characteristics of each group are presented in Table I. The 3 groups were well matched for age, height, weight and body mass index (BMI).
Fig. 1. (a) Assessment of the medial tibiofemoral (TF) osteoarthritis (OA) by anteroposterior radiographic view of a knee. (b) Group A: medial TF osteoarthritic knee with normal patellar alignment. (c) Group B: medial TF osteoarthritic knee with patellar malalignment.
| Table I. Characteristics of the participants |
| | Group A | Group B | Group C |
| Sex, men/women (n) | 3/8 | 5/9 | 3/7 |
| Age (years), mean (SD) | 61.1 (10.3) | 63.4 (11.0) | 61.4 (6.5) |
| Height (cm), mean (SD) | 156.0 (9.8) | 162.0 (6.2) | 157.0 (8.5) |
| Weight (kg), mean (SD) | 59.7 (9.3) | 65.3 (10.5) | 57.8 (9.9) |
| BMI, mean (SD) | 24.4 (2.4) | 24.8 (4.3) | 23.2 (2.2) |
| Lequesne’s Index*, mean (SD) | 6.91 (3.88) | 6.1 (3.26) | |
| *Lequesne Index (16) was used to assess the severity of osteoarthritis affecting the knee joint through evaluation of daily activity and function. The relationship of this index to the common measure of handicap is as follows: (i) more than 13: extremely severe; (ii) 11–13: very severe; (iii) 8–10: severe; (iv) 5–7: moderate; (v) 1–4: minor. SD: standard deviation; BMI: body mass index. |
Procedures
Isokinetic concentric assessment of knee extensor muscles was evaluated using a Cybex Norm (Cybex International Inc., Medway, MA, USA) dynamometer. The subjects were in the seated position on the Cybex dynamometer, with their back supported and the hips flexed to 85°, as this is a good position for testing both the extensors and flexors (17). Trunk and thigh straps were fastened for stabilization. The range of angular movement of the knee joint was from 90° to 0° and the test velocities were 80°, 120° and 240°/sec. Before the test, each subject was warmed up by walking for 10 min and practiced at submaximal contraction levels, and then rested for 5 min in a sitting position. The testing consisted of a series of 5 repetitive isokinetic concentric contractions from 90° (flexion) to 0° (extension) at each velocity. The sequences of the applied velocities were 80°, 120° and 240°/sec. All of the subjects were encouraged, using visual feedback, to perform maximal contractions.
EMG analysis
BIOPAC MP100 (BIOPAC Systems Inc., Goleta, CA, USA), a system with 6 channels was used to collect the EMG signals. The amplitude of muscle activities were recorded on 2 channels. Other channels were used to record the signals for angular velocity, direction (flexion/extension), torque and position (degree of knee extension), respectively. After skin preparation with isopropyl alcohol, bipolar gold-plated surface electrodes were centred on the muscle bellies of the VMO and distal VL, as described by Basmajian & Blumenstein (18). The inter-electrode distance was 3 cm. The ground electrode was placed over the tibial tubercle. Following the knee extension trials, the peak muscle torque and EMG activity were recorded. Data were collected at 1000 Hz and then stored using AcqKnowledge software (Version 3.7.3) on a personal computer and later analysed with custom LabVIEW software (Version 7.1, National Instruments Corporation, Austin, TX, USA). The raw EMG data was processed by generating the EMG linear envelope method. Signals were band-pass filtered (20–500Hz), full-wave rectified and finally smoothed at 6 Hz using a low-pass second-order Butterworth digital filter. The peak amplitude of filtered EMG signal for the VMO and VL was presented as the VMO/VL ratio. The VMO/VL ratios were averaged by 3 extension cycles (excluding the first and fifth cycle) during each velocity trial. A ratio of less than 1 indicated that the EMG signal activity for the VMO was lower than that of the VL.
Image analysis
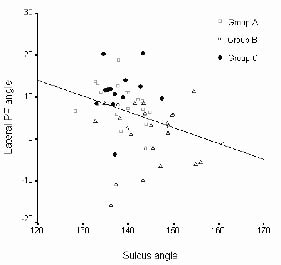
The bony characteristics of PFJ of each patient were measured using a Merchant’s view radiograph (Fig. 2) (19, 20). Trochlear depth was measured by the sulcus angle (Fig. 2a, ∠ABC). In the normal knee (19), the averaged sulcus angle was 138° (range 126–150°). The congruence angle, which is used to measure the relationship of the patellar articular ridge to the groove of the femoral trochlear (Fig. 2a), was defined by Merchant et al. (15). The normal congruence angle has a negative value. A positive value or greater than +16° is considered to be abnormal and indicates lateral instability of the patella (15, 19). Patellar tilting was measured by the lateral PF angle (Fig. 2b). Angles that are smaller than 7° or negative (medial opening) indicate an abnormal situation and a lateral tilt (21). The method of measuring lateral patellar displacement (%) has been described by Keblish et al. (22) and is shown in Fig. 2c.
Fig. 2. Measurement of the patellofemoral joint (PFJ) anatomy. (a) Sulcus angle (∠ABC) and congruence angle (α). The congruence angle is measured between the bisector line of sulcus angle and a line joining the apex of the point B and the lowest point of the patellar articular surface D; (b) lateral patellofemoral angle (β) (19); (c) perpendicular lines (AA′, BB′ and DD′) were dropped to a horizontal line. Percentage of lateral patellar displacement (%) was defined by the ratio A′D′/A′B′. The ratio for normal tracking is approximately 100% (21).
Statistical analysis
Non-parametric Kruskal-Wallis one-way analysis of variance (ANOVA) was used for comparison of average VMO/VL EMG ratios and anatomical parameters between the 3 groups. A least significant difference criterion was used to judge the significance of post hoc tests. The Pearson correlation analyses were performed to determine the relationship between PFJ structure and the VMO/VL EMG ratio. Subjects from all 3 groups were grouped together for this analysis. The post hoc power analysis was used to analyse retrospectively the power of an observed effect of the sample size and make an estimate of parameters derived from a given data-set (23). Statistical analysis was performed with SPSS Version 10.0. The alpha level for the ANOVA was 0.05.
Results
Peak muscle torque and VMO/VL EMG ratios
The peak muscle torques of both group A and group B had smaller values than group C (p < 0.05) (Table II), but there were no significant differences between groups A and B for all the 3 tested velocities (p > 0.05).
The VMO/VL EMG ratios of group B were averaged 0.76 (standard deviation (SD) 0.15) at an angular velocity of 80°/second, 0.81 (SD 0.22) at the 120°/second and 0.84 (SD 0.24) at the 240°/second, all of which were lower than the corresponding results for group A and group C (p < 0.05, Table II). No difference in the VMO/VL ratios was noted between group A and group C; both of them were closed to 1.0. There was no significant effect of the testing velocities on the VMO/VL EMG ratios across any of the groups (p > 0.05).
| Table II. Comparison of the peak muscle torque and vastus medialis oblique (VMO) / vastus lateralis (VL) electromyographic ratios between the 3 groups during knee isokinetic testing (means with standard deviation in parentheses) |
| | Group A | Group B | Group C | p-value |
| Peak muscle torque (%BW) |
| 80°/sec | 40.0 (13.7)* | 39.7 (14.0)† | 64.4 (6.8) | < 0.001 |
| 120°/sec | 33.6 (11.8)* | 35.6 (13.3)† | 57.1 (6.4) | < 0.001 |
| 240°/sec | 23.7 (8.4)* | 24.7 (9.8)† | 44.1 (8.6) | < 0.001 |
| EMG of the VMO/VL ratio |
| 80°/sec | 0.96 (0.27) | 0.75 (0.14)†,‡ | 0.91 (0.12) | 0.001 |
| 120°/sec | 0.96 (0.23) | 0.81 (0.23)†,‡ | 0.94 (0.15) | 0.037 |
| 240°/sec | 1.00 (0.22) | 0.84 (0.23)†,‡ | 0.96 (0.16) | 0.031 |
| *Significant difference between group A and group C (p < 0.05). †Significant difference between group B and group C (p < 0.05). ‡Significant difference between group A and group B (p < 0.05). EMG: electromyography; BW: body weight. |
Image analysis
The radiographic parameters of the PFJ structure are presented in Table III. The mean sulcus angle in group B (144.8 (SD 7.37)) was significantly larger than in group A (138.5 (SD 4.68)), p < 0.001. The mean congruence angle, lateral PFJ angle and percentage of lateral patellar displacement in group B were all significantly different compared with group A and with group C (p < 0.05), which indicated that the patella was not drawn into the trochlear groove in patients with patellar malalignment.
| Table III. Comparison of radiographic parameters between the 3 groups. |
| | Group A Mean (SD) range | Group B Mean (SD) range | Group C Mean (SD) range | ANOVA p-value |
| Sulcus angle (°) | 138.5 (4.68) 128.4~144.8 | 144.8 (7.37)* 132.7~160.9 | 138.2 (4.07) 133.1~147.4 | 0.001 |
| Congruence angle (º) | –4.61 (9.11) –20.89~10.16 | 14.66 (20.34)* –13.64~55.24 | –4.80 (17.77) –43.9~17.2 | 0.001 |
| Lateral PF angle (º) | 9.03 (4.04) 1.88~18.71 | 1.41 (6.81)* –15.77~11.3 | 11.20 (5.91) –3.66~20.43 | < 0.001 |
| Percentage of lateral patellar displacement (%) | 103.7 (9.32) 78.7~124.4% | 91.3 (9.99)* 71.2~109.6% | 101.5 (7.65) 92.2~118% | < 0.001 |
| *Group B was significantly different from group A and group C at p < 0.05. ANOVA: analysis of variance; PF: patellofemoral; SD: standard deviation. |
Relationship between EMG ratios and patellar bony structure
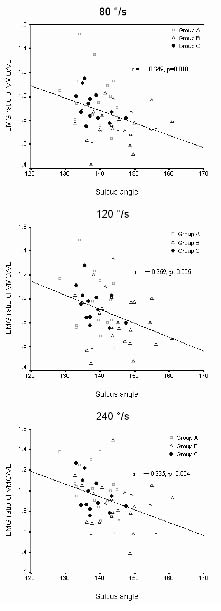
Pearson’s correlation coefficients were obtained for the relationship between the sulcus angle and lateral PFJ angle across all knees (r = –0.335, p = 0.013, observed power was 0.74) (Fig. 3). The sulcus angle was negatively correlated with patellar tilt and as the sulcus angle increased, the amount of lateral PFJ angle (α) decreased. All of the EMG ratios of VMO/VL were found to be correlated with the sulcus angle at 80°/sec, 120°/sec and 240°/sec (Table IV, Fig. 4), the post hoc power analysis were 0.59, 0.83 and 0.86, respectively. There were no correlations between EMG and congruence angle, lateral PFJ angle and percentage of lateral displacement (p > 0.05).
Fig. 3. There was a negative correlation between lateral patellofemoral (PF) angle and sulcus angle (r = –0.335, p = 0.013).
| Table IV. Pearson correlation coefficients (r) for electromyographic (EMG) ratios and radiographic parameters |
| EMG ratio of VMO/VL | 80°/sec | 120°/sec | 240°/sec |
| Sulcus angle (°) | r = –0.349* p = 0.010 | r = –0.369* p = 0.006 | r = –0.385* p = 0.004 |
| Congruence angle (°) | r = –0.150 p = 0.28 | r = –0.038 p = 0.787 | r = –0.056 p = 0.686 |
| Lateral PF angle (°) | r = 0.268 p = 0.050 | r = 0.306* p = 0.024 | r = 0.208 p = 0.132 |
| Lateral patellar displacement (%) | r = 0.165 p = 0.233 | r = 0.027 p = 0.847 | r = 0.060 p = 0.665 |
| *Correlation is significant at the 0.05 level (2-tailed). VMO: vastus medialis oblique; VL: vastus lateralis; PF: patellofemoral. |
Fig. 4. All the electromyographic (EMG) ratios were negatively correlated with the sulcus angle at 80°/sec, 120°/sec and 240°/sec.
Discussion
Clinically, patellar malalignment is a common occurrence in patients with osteoarthritic knee. Our results showed that both patients with osteoarthritic knees in group A (with normal patellar alignment) and group B (with patellar malalignment) had lower quadriceps torques compared with healthy subjects in group C (p < 0.001); however, no difference was found in quadriceps torque between groups A and B. When compared with groups A and C, group B had a significant reduction in the VMO/VL ratio (VMO/VL ratio < 1), which exhibited an imbalance in muscle activities of the VMO and VL. In contrast to group B, the VMO/VL EMG ratios of group A patients were all almost 1, which was similar to the healthy subjects. These results suggested that deficiency of the VMO or excessive pull of the VL on the patella might cause abnormal patellar tracking of the extensor mechanism in osteoarthritic subjects with patellar malalignment.
Results of morphology of the PFJ revealed significant differences between osteoarthritic subjects with and without patellar malalignment; in particular, the sulcus angle showed a larger value in osteoarthritic subjects with patellar malalignment. Fucentese et al. (24) suggested that a larger sulcus angle might have a genetic origin, such as insufficient trochlear depth and decreased lateral trochlear slope occurring in trochlear dysplasia. Another measure of patellar tracking in this study was lateral PF angle, the data showed that subjects of group B had rather laterally patellar tilting compared with groups A and C. Moreover, the sulcus angle was significantly correlated with the lateral PF angle. This finding seems to imply that a larger sulcus angle may lead to more patellar tilting and compromised patellar stability.
In addition, the sulcus angle was significantly correlated with the EMG ratio for all isokinetic knee extension tasks, although the correlation coefficients were not high (r = –0.349 ~ –0.385, p < 0.05). It is apparent that the increase in the sulcus angle is related to a decrease in the EMG ratio, which may cause the muscle imbalance of VMO and VL. From a biomechanical view, the dynamic position of the patella is dependent on the vectors of the quadriceps muscle group (19). In the terminal 30° from flexion to extension, the “screw home” mechanism rotates the tibia outward relative to the femur, displacing the tibial tuberosity laterally and increasing the quadriceps angle, with the result that a lateral vector is created acting on the patella. At this moment, the VMO and medial retinaculum tend to resist the lateral vector, and the lateral facet of the trochlear also limits patellar lateral subluxation. For this reason, the VMO muscle and the lateral facet of the trochlear seem to play an important role in stabilizing the kinetics of the patella (10, 19) Our results were also consistent with the findings of Powers (11), who reported that subjects with PFPS had a larger sulcus angle, from 45° to 0° of knee flexion. Powers (11) suggested that the sulcus angle might be an important determinant of patellar kinetic movement at end-range of knee extension, but the EMG activity of the VMO/VL muscles did not appear to be correlated with abnormal patellar tracking. The EMG activation pattern was different from our finding. These differences might be due to the experimental settings of the knee extension device. A prone position and isotonic contraction of knee flexion were used in Powers’ study.
The results may have an impact on the prescription of rehabilitation treatments, such as muscle strength training strategy, for patients with OA. Strengthening of the quadriceps is a main rehabilitative strategy for patients with osteoarthritic knee. Isokinetic exercise is one of the effective and well-tolerated treatments for patients with osteoarthritic knee. However, it is necessary to identify the type of osteoarthritic knee. Merchant’s view radiography may be a routine assessment and this will help to distinguish patients with OA knee into 2 groups. In patients with osteoarthritic knee with patellar malalignment, the selection of specific muscle for the strengthening programme is essential for restoration of dynamic patella stability. For example, Laprade et al. (25) demonstrated that isometric exercise, such as knee extension combined with medial tibial rotation, appears to increase the VMO/VL ratio. Tang et al. (9) found that a closed kinetic chain exercise from 0° to 60° of knee flexion could induce maximal VMO firing. These types of therapeutic exercises may be more beneficial in OA knee patients with patellar malalignment. However, larger sample sizes should be needed to verify the effectiveness of these rehabilitative strategies in the future.
There were several limitations to this study. Regarding EMG analysis, the absolute EMG amplitudes were influenced by physical and physiological phenomena including muscle contraction force, muscle fibre length, muscle volume, skin impedances, and recruitment stability (26). With use of VMO/VL ratios, the variation of individuality causes by the aforementioned influencing factors can be reduced; in addition, different performance of VMO and VL in each tested subject can be clearly observed. Although the VMO/VL ratio cannot denote the actual force generated by these muscles, it can help us to understand the contribution of these 2 muscles during quadriceps contraction.
In this study, we took the radiograph at 45° of knee flexion; the patellar was engaged fully with the trochlear groove in this position (19). It is useful to determine subluxation, joint space narrowing and patellar deformity. However, the limitation of this technique is that it provides only a static picture of extensor mechanism in a supine patient, but cannot reflect the morphology and relative position of patella and trochlear groove through the total range of motion during dynamic knee flexion. In Farahmand et al’s findings (10), the trochlear groove geometry changed very little with progressive knee flexion. Besides the relationship between muscle contraction and morphology of the femoral trochlear, tightness of soft tissues such as the lateral retinaculum and iliotibial band may also be factors involved in malalignment and pathology of the PFJ (4). Further research is needed into whether other factors can help us to explore more about patellar kinematics.
In conclusion, a larger sulcus angle of the patellofemoral joint was found in subjects with osteoarthritic knee with patellar malalignment, and this may be an important factor causing imbalance in muscle activities of the VMO and VL during quadriceps contraction.
References
1. Harrison MM, Cooke TD, Fisher SB, Griffin MP. Patterns of knee arthrosis and patellar subluxation. Clin Orthop Rel Res 1994; 309: 56–63.
2. Inaba Y, Numazaki S, Koshino T, Saito T. Provoked anterior knee pain in medial osteoarthritis of the knee. Knee 2003; 10: 351–355.
3. Dalury DF. Total knee replacement for patellofemoral disease. J Knee Surg 2005; 18: 274–277.
4. Grelsamer RP. Patellar malalignment. J Bone Joint Surg 2000; 82A: 1639–1650.
5. Fulkerson JP, editor. Disorders of the patellofemoral joint. 3rd edn. Baltimore: Williams & Wilkins; 1997, p. 175–196.
6. Arendt E. Anatomy and malaignment of the patellofemoral joint. Its relation to patellofemoral arthrosis. Clin Ortho Rel Res 2005; 436: 71–75.
7. Sakai N, Luo ZP, Rand JA, An KN. The influence of weakness in the vastus medialis oblique muscle on the patellofemoral joint: an in vitro biomechanical study. Clin Biomech 2000; 15: 335–339.
8. Souza DR, Gross MT. Comparison of vastus medialis obliquus: vastus lateralis muscle integrated electromyographic ratios between healthy subjects and patients with patellofemoral pain. Phys Ther 1991; 71: 310–316.
9. Tang SFT, Chen CK, Hsu R, Chou SW, Hong WH, Lew HL. Vastus medialis obliquus and vastus lateralis activity in open and closed kinetic chain exercises in patients with patellofemoral pain syndrome: an electromyographic study. Arch Phys Med Rehabil 2001; 82: 1441–1445.
10. Farahmand F, Senavongse W, Amis AA. Quantitative study of the quadriceps muscles and trochlear groove geometry related to instability of the patellofemoral joint. J Ortho Res 1998; 16: 136–143.
11. Powers CM. Patellar kinetics part II: the influence of depth of the trochlear groove in subjects with and without patellofemoral pain. Phys Ther 2000; 80: 965–973.
12. Cooper C, McAlindon TE, Snow S. Mechanical and constitutional risk factors for symptomatic knee osteoarthritis: differences between medial tibiofemoral and patellofemoral disease. J Rheumatol 1994; 21: 307–313.
13. Baker KR, Xu L, Zhang Y, Nevitt M, Niu J, Aliabadi P, et al. Quadriceps weakness and its relationship to tibiofemoral and patellofemoral knee osteoarthritis in Chinese. Arthritis Rheum 2004; 50: 1815–1821.
14. Ahlback S. Osteoarthrosis of the knee: a radiographic investigation. Acta Radiol Suppl 1968; 277: 7–72.
15. Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg 1974, 56A: 1391–1396.
16. Lequesne MG. The algofunctional indices for hip and knee osteoarthritis. J Rheumatol 1997; 24: 779–781.
17. Dvir Z, editor. Isokinetics: muscle testing, interpretation, and clinical applications. Edinburgh: Churchill Livingstone; 1994, p. 101–128.
18. Basmajian JV, Blumenstein R, eitors. Electrode placement in EMG biofeedback. Baltimore: Williams & Wilkins; 1980.
19. Egund N, Ryd L. Patellar and quadriceps mechanism. In: Davies AM, editor. Imaging of the knee, 1st edn. Berlin: Springer–Verlag; 2002, p. 217–248.
20. Eliasa DA, White LM. Imaging of patellofemoral disorders. Clin Radiol 2004; 59: 543–557.
21. Laurin CA, Levesque HP, Dussault R, Labelle H, Peides JP. The abnormal lateral patellofemoral angle. A diagnostic roentgenographic sign of recurrent patellar subluxation. J Bone Joint Surg 1978; 60A: 55–60.
22. Keblish PA, Varma AK, Greenwald AS. Patellar resurfacing or retention in total knee arthroplasty. A prospective study of patients with bilateral replacements. J Bone Joint Surg 1994; 76B: 930–937.
23. Soper DS. Post-hoc statistical power calculator. [Accessed 2007]. Available from: http://www.danielsoper.com/statcalc
24. Fucentese SF, Roll AV, Koch PP, Epari DR, Fuchs B, Schottle PB. The patella morphology in trochlear dysplasia – a comparative MRI study. Knee 2006; 13: 145–150.
25. Laprade J, Culham E, Brouwer B. Comparison of five isometric exercises in the recruitment of the vastus medialis oblique in persons with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther 1998; 27: 197–204.
26. Luca CJD. The use of surface electromyography in biomechanics. J Appl Biomech 1997; 13: 135–163.