OBJECTIVE: To explore physical and psychological measures believed to determine patients’ perceived self-efficacy in the rehabilitation of patients with anterior cruciate ligament injury.
DESIGN: An explorative descriptive study.
Patients: A total of 116 patients with an anterior cruciate ligament deficient or reconstructed knee.
Method: At one visit; 12 months post-injury/reconstruction, patients reported their perceived self-efficacy on the Knee Self-Efficacy Scale. Thirty-nine other measures related to self-efficacy were also documented. A linear regression model was applied to identify determinants of perceived self- efficacy.
RESULTS: 40% of the variance in the complete Knee Self- Efficacy Scale was explained by the Lysholm score, Knee Injury and Osteoarthritis Outcome ScoreSport/Recreation, Internal Locus of Control and Locus of Control by Chance. The variance in patients’ present perceived self-efficacy was explained to 41% by the same measures. Perceived self-efficacy of future capability was explained to 38% by the variance in the Lysholm score, Knee Injury and Osteoarthritis Outcome ScoreSport/Recreation, TegnerPresent level and Internal Locus of Control.
CONCLUSION: Self-reported symptoms/functions and Internal Locus of Control were the most important determinants of self-efficacy in patients with an anterior cruciate ligament injury. In order to strengthen self-efficacy, these determinants should be considered by the clinicians involved in the rehabilitation.
Key words: coping strategies, locus of control, symptoms and physical functioning, K-SES, self-efficacy.
J Rehabil Med 2007; 39: 486–492
Correspondence address: Pia Thomeé, Lundberg Laboratory for Orthopaedic Research, Gröna Stråket 12, Sahlgrenska University Hospital, SE-413 45 Göteborg, Sweden. E-mail: pia.thomee@orthop.gu.se
Submitted July 30, 2006; accepted February 14, 2007
*This article has been fully handled by one of the Associate Editors, who has made the decision for acceptance.
Introduction
Self-efficacy beliefs are said to influence not only the individual’s course of action, but also the effort they expend, their endurance in the face of difficulties, the nature of their thought patterns and their affective reactions (1). Self-efficacy is task specific and can, for example, be applied to functional, social and academic tasks.
Little is known about the factors that make up self-efficacy for patients with an anterior cruciate ligament (ACL) injury. Self-efficacy is strongly related to clinically significant improvements in performance for patients with an ACL injury (2). To understand what factors relate to self-efficacy may therefore help us to improve the results of rehabilitation. To our knowledge, determinants of self-efficacy have not been studied in patients with an ACL injury. The determinants of self-efficacy for physical tasks have, however, been studied in patients with other knee-related problems (3). For patients with osteoarthritis of the knee, 51% of the variance in functional self-efficacy was explained by self-reported knee stiffness, age, depression scores and hamstring strength in community-dwelling adults who were 50 years of age or more (3).
Using the Knee Self-Efficacy Scale (K-SES), a new valid and reliable instrument, it is now possible to study self-efficacy in patients with an ACL injury (4). The K-SES has also been shown to be sensitive to clinically relevant changes, i.e. the K-SES has good responsiveness, when it comes to self-efficacy during the rehabilitation of patients with an ACL injury (2).
It has been suggested that how well a person performs is predicted better by that person’s beliefs about him/herself and his/her capabilities than by what he/she is actually capable of accomplishing (5). Factors associated with emotional responses to injury are: perceived quality of life, perception of health locus of control, and strategies used to cope with the injury (6). Patients with a knee injury who use negative coping strategies in terms of pain and report a poorer quality of life, have been shown to have an inferior result after rehabilitation and surgery (7, 8). Patients with an ACL injury have been shown to have less perceived functional limitations when they believe that their health status is directly related to their own behaviour, i.e. controlled by internal locus (9).
Perceived self-efficacy has also been shown to be important for the understanding of both psychological and physical function in patients with rheumatic disease, as well as for patients with whiplash-associated disorders (WAD) (10–12). An injury to the ACL can be compared to an injury resulting in WAD, in terms of being sudden, unpredictable and devastating for the patient.
We hypothesize that patients’ perceived self-efficacy may be determined by factors such as coping with pain and locus of control, as well as previous experience of injuries/illness, quality of life, symptoms and physical function one year after ACL injury/reconstruction.
The purpose of this study was to explore physical and psychological measures believed to determine patients’ perceived self-efficacy in the rehabilitation of patients with an ACL injury.
These possible determinants may help to provide a better understanding of some of the underlying factors characterizing self-efficacy and to improve strategies in rehabilitation for patients with an ACL injury.
Material and methods
Subjects
A total of 116 patients with a mean age of 31.2 years (range 18–55 years) were included in the study. Forty-five patients (49% women) had an ACL-deficient knee and 71 patients (34% women) had undergone an ACL reconstruction. All patients were recruited consecutively for a prospective study within one month after injury or within one month before scheduled surgery. For the present 1-year follow-up study, the following inclusion criteria had to be fulfilled: ACL injury based on history and a clinical examination performed by an experienced orthopaedic surgeon, age in the range 18–60 years, ACL injury or ACL reconstruction one year prior to testing, injured during sports activity (Tegner activity level 3–10), rehabilitated for at least 3–6 months at a sports rehabilitation clinic and able to read and understand Swedish.
The study was approved by the Human Research Ethics Committee at the Faculty of Medicine, Göteborg University, Sweden. Written informed consent was obtained and the rights of subjects were protected.
Procedure
All the data were documented at one visit to the laboratory, 12 months after injury/reconstruction. The questionnaires/outcome measures were self-administered according to recommended procedures using the SF-36 Swedish manual and interpretation guide (13). Data were missing for present Physical Activity Scale (PASPresent) for 2 patients and for present physical activity level (TegnerPresent) for one patient. One experienced physical therapist collected and scored all the questionnaires/outcome measures.
K-SES – the dependent measure for self-efficacy
The K-SES is a self-administered, valid and reliable instrument (4) with good responsiveness (2). The K-SES comprises 22 items in 4 sections. For sections A; Daily activities (7 items), B; Sports activities (5 items) and C; Knee function tasks (6 items), the patients report how certain they are about performing the task right now, despite knee pain/discomfort. For section D; Knee function in the future (4 items), the patients report how certain they feel about their future capabilities. Patients give their responses to the 22 items using an 11-grade Likert scale, ranging from 0 = not at all certain about the task to 10 = very certain about the task. The sum of the item scores is calculated and divided by the number of items. Because of 2 strong factors identified by a factor analysis of the K-SES, separate analyses were made of sections A, B and C, for present physical performance/function (factor 1), and of the D section, how the patients perceived the future physical performance/prognosis of their knee (factor 2) (4).
Independent measures
Thirty-nine independent measures (IM), being possible determinants of self-efficacy, were documented with several self-administrated questionnaires (scores) or psychological instruments and were grouped into: Present Personal Factors (IM 1–25), Previous Experience Factors (IM 26–31) and Symptom and Function Factors (IM 32–39). The grouping was performed by the researchers and was categorized on the basis of quality factors.
Present personal factors
Demographics. Patients were documented for gender (IM 1) and whether or not they had undergone reconstructive surgery (IM 2). Patients’ intensity and frequency of participation in physical activity were documented using the Physical Activity Scale (PAS) at present (PASPresent) (IM 3) (2). Patients also reported their present physical activity level (TegnerPresent) (IM 4) on the Tegner activity grading scale (14). The patients’ ages (IM 5) were also documented.
The PAS was constructed using a validated score for middle-aged and former athletes as a model (15). An expert group consisting of experienced physical therapists and orthopaedic surgeons assured the good face validity of the new scale. On the PAS, subjects made their own assessment of how vigorously and frequently they participated in physical activity at the present time and prior to their knee injury. The 4 grades in the PAS were:
1. Non-active, only sometimes going for a short walk or doing light work in the garden or similar.
2. Light physical activity a few hours a week, such as taking a long walk, bicycling, dancing, normal gardening, or similar.
3. More strenuous physical activity a few hours a week, such as playing tennis, swimming, running, workout, spinning, dancing, football, indoor hockey, strenuous gardening, or similar.
4. Hard strenuous physical activity during the week on a regular basis, requiring demanding effort.
The Tegner scale has good reliability for grading work and sport activities (14). It is numerically graded from 1 to 10; 1 represents the least strenuous knee activity and 10 is hard strenuous knee activity, such as rugby or international soccer. The Tegner scale was modified in 2000 (not yet published) and the modified version was used in this study with the permission of the authors (Tegner, personal communication).
Psychosocial variables. Present health-related quality of life was assessed using the SF-36 (IM 6–13) and coping strategies were assessed using the Coping Strategies Questionnaire (CSQ) (IM 14–22) (16, 17). Locus of control was documented with the Multidimensional Health Locus of Control (MHLC) (IM 23–25) (18).
The SF-36 is a valid and reliable health-related quality of life instrument (16). It consists of 36 items divided into 8 dimensions: Physical Functioning, Role-Physical, Bodily Pain, General Health, Vitality, Social Functioning, Role-Emotional and Mental Health.
The CSQ is a valid and reliable questionnaire to assess coping strategies for pain (17). It is a self-administrated instrument forming 7 cognitive coping strategies. The strategies are: Diverting Attention, Re-interpreting Pain Sensations, Coping Self-Statement, Ignoring Sensations, Praying/hoping, Catastrophizing, Increased Behavioural Activities. Two additional items reflects how the patients feel about their perceived ability to control or reduce their pain: Control Pain and Decrease Pain. The Swedish version of the CSQ was used in the present study (19).
The MHLC is a valid and reliable measure of people’s beliefs that their health is or is not determined by their behaviour (18). The “internal health locus of control” refers to the individual’s belief that their own behaviour is directly related to outcome. The “external health locus of control” refers to the individual’s belief that their outcome after injury or surgery is under the control of powerful others and the “health locus of control by chance” refers to the individual’s belief that their outcome is determined by fate, luck or chance. The Swedish version of the MHLC was used with the permission of Professor Sven Carlsson (Department of Psychology, Göteborg University), who performed the translation and cross-cultural adaptation.
Previous experience factors
Previous injury/illness. Previous injuries (InjuryPrevious) or previous illnesses (IllnessPrevious) were documented as the number of serious injuries (IM 26) and illnesses (IM 27) the patients could recall having had. Serious injury was defined as any injury/illness that resulted in surgery and/or rehabilitation for more than 2 months. The subjects also documented whether they had no, good or bad experience of their injury (InjuryExperience) or illness (IllnessExperience) when resuming their prior physical activity (IM 28–29) – good experience = resumed prior physical activity within 6 months and bad experience = did not resume prior physical activity or needed more than 6 months before resuming prior physical activity.
Previous physical activity. The PAS was used to describe the intensity and frequency of participation in physical activity prior to the ACL injury (PASPre-injury) (IM 30), while the Tegner activity grading scale was used to document the subjects’ physical activity level prior to their ACL injury (TegnerPre-injury) (IM 31) (14).
Symptom and function factors
Physical activity. How well the subjects had resumed the intensity and frequency of participation in physical activity was documented using the PAS (PASResumed) (IM 32), and how well they had resumed their prior physical activity level was documented using the Tegner scale (TegnerResumed) (IM 33). To be considered as having resumed baseline PAS, the grade of activity had to be unchanged or improved. The subjects were considered to have resumed their baseline physical activity level if they reported improved, unchanged or 1 level lower on the Tegner scale.
Symptoms. Subjective knee symptoms and functions were documented by the Knee Injury and Osteoarthritis Outcome Score (KOOS) (IM 34–38) and the Lysholm score (IM 39) (20, 21).
The KOOS is a valid and reliable self-administered instrument with good responsiveness for assessing knee function, symptoms and associated problems for patients with a knee injury (20). It consists of 5 subscales; pain, symptoms, function in daily living, function in sports and recreation, and knee-related quality of life.
The Lysholm score is a valid and reliable symptom-related knee score (21). It measures 8 symptoms and the specific disability for that symptom. In the present study, the patients assessed their symptoms themselves.
Statistical analysis
Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS, version 14.0 for Windows). Standard procedures were used for descriptive statistics. All correlation coefficients (rs) were calculated using Spearman’s rank correlation. Significance was considered at the α level of p < 0.05. For the linear regression analysis, the K-SES score was transformed to normal scores by the transformation by Blom. All the bivariate correlations between the K-SES and the independent measures with a p-value of < 0.05 were used in the forward stepwise linear regression model.
Results
Self-efficacy
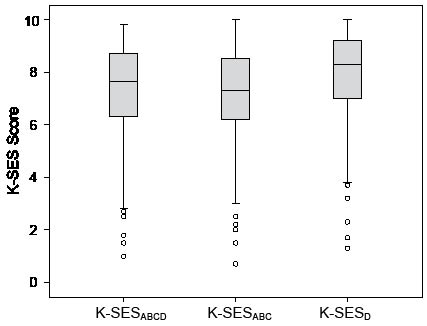
For the 116 patients, the mean (standard deviation (SD)) for the complete K-SES (K-SESABCD) was 7.3 (1.9) and the scores ranged from 1.0 to 9.8. The mean (SD) for the K-SESABC was 7.1 (2.0), ranging from 0.7 to 9.8 and for the K-SESD it was 7.8 (1.9), ranging from 1.3 to 10. The median and interquartile range for K-SES are illustrated in Fig. 1.
Fig. 1. Median, 5th, 25th, 75th and 95th percentiles and outliers for the perceived self-efficacy (K-SES) for 116 patients one year after anterior cruciate ligament reconstruction.
Determinants
Descriptive statistics for the 39 IMs, Present Personal Factors (IM 1–25), Previous Experience Factors (IM 26–31) and Symptoms and Function Factors (IM 32–39), are presented in Tables I (a and b). The study population comprised typically active people with an ACL injury, with normal means for the Lysholm score and the 5 dimensions on the KOOS and ranging in physical activity level from 3 to 10 on the Tegner activity scale. There were only a few missing data, 2 on PASPresent and one on TegnerPresent.
| Table I (a). Values for the present personal factors (IM 1–25). |
| Factors | n | Mean (SD) | Med (IQR) | Min (Max) |
| 1. Gender, | | | | |
| Female/ Male | 46/70 | | | |
| 2. Surgery, | | | | |
| Yes/No | 71/45 | | | |
| 3. PASPresent† | | | | |
| 1st grade | 3 | | | |
| 2nd grade | 30 | | | |
| 3rd grade | 63 | | | |
| 4th grade | 18 | | | |
| 4. TegnerPresent* | | 5.2 (0.2) | 5 (3) | 1 (10) |
| 5. Age (years) | | 31.3 (8.9) | 30 (14) | 18 (55) |
| SF-36 | | | | |
| 6. Physical Functioning | | 82.4 (19.0) | 90 (20) | 5 (100) |
| 7. Role – Physical | | 73.5 (38.4) | 100 (50) | 0 (100) |
| 8. Bodily Pain | | 76.3 (21.9) | 84 (38) | 2 (100) |
| 9. General Health | | 82.0 (17.0) | 87 (22) | 25 (100) |
| 10. Vitality | | 54.0 (9.2) | 54 (10) | 35 (85) |
| 11. Social Functioning | | 87.8 (18.5) | 100 (25) | 25 (100) |
| 12. Role – Emotional | | 79.1 (35.2) | 100 (33) | 0 (100) |
| 13. Mental Health | | 66.1 (7.9) | 64 (12) | 48 (88) |
| CSQ | | | | |
| 14. Diverting Attention | | 2.2 (1.4) | 2 (2) | 0 (5) |
| 15. Reinterpreting Pain | | 1.2 (1.3) | 1 (2) | 0 (6) |
| 16. Coping | | 3.8 (1.4) | 4 (2) | 0 (6) |
| 17. Ignoring | | 2.8 (1.5) | 3 (2) | 0 (6) |
| 18. Praying | | 1.8 (1.2) | 2 (1) | 0 (6) |
| 19. Catastrophizing | | 2.1 (1.0) | 2 (2) | 0 (4) |
| 20. In Behaviour | | 2.4 (1.0) | 2 (1) | 0 (5) |
| 21. Controlling Pain | | 4.8 (1.2) | 5 (2) | 0 (6) |
| 22. Decreasing Pain | | 4.0 (1.3) | 4 (2) | 0 (6) |
| MHLC | | | | |
| 23. Internal Locus of Control | | 3.9 (0.8) | 3.8 (1.2) | 1.8 (5.5) |
| 24. External Locus of Control | | 2.4 (0.7) | 2.3 (0.8) | 1.0 (4.8) |
| 25. Chance Locus of Control | | 2.4 (0.8) | 2.4 (1.3) | 1.0 (4.7) |
| n: frequency; SD: standard deviation; med: median; IQR: interquartile range; Min: minimum; Max: maximum; IM: independent measures; MHLC: Multidimensional Health Locus of Control; CSQ: Coping Strategies Questionnaire. *1 missing, †2 missing, PAS: Physical Activity Scale. |
| Table I (b). Values for the earlier experience factors (IM 26–31) and symptom and function factors (IM 32–39). |
| Factors | n | Mean (SD) | Med (IQR) | Min (Max) |
| Values for the earlier experience factors |
| 26. InjuryPrevious | | | | |
| Yes/No | 72/44 | | | |
| 27. IllnessPrevious | | | | |
| Yes/ No | 39/77 | | | |
| 28. InjuryExperience | | | | |
| None | 44 | | | |
| Good | 42 | | | |
| Bad | 30 | | | |
| 29. IllnessExperience | | | | |
| None | 77 | | | |
| Good | 31 | | | |
| Bad | 8 | | | |
| 30. PASPre-injury, | | | | |
| 1st grade | 0 | | | |
| 2nd grade | 13 | | | |
| 3rd grade | 57 | | | |
| 4th grade | 46 | | | |
| 31. TegnerPre-injury | | 7.1 (1.9) | 7 (2) | 3 (10) |
| Values for the symptom and function factors (IM 32–39) |
| 32. PASResumed | | | | |
| Yes/No | 65/ 49 | | | |
| 33. TegnerResumed | | | | |
| Yes/No | 57/ 58 | | | |
| 34. KOOSSymptoms | | 90.9 (9.6) | 93 (10) | 44 (100) |
| 35. KOOSPain | | 85.3 (11.9) | 89 (14) | 43 (100) |
| 36. KOOSAd | | 96.0 (6.4) | 99 (4) | 68 (100) |
| 37. KOOSSports/Recreation | | 77.7 (18.0) | 85 (24) | 0 (100) |
| 38. KOOSQoL | | 67.7 (17.9) | 69 (25) | 12 (100) |
| 39. Lysholm score | | 85.3 (10.4) | 86 (16) | 57 (100) |
| n: frequency; SD: standard deviation; med: median; IQR: interquartile range; Min: minimum; Max: maximum; IM: independent measures. PAS: Physical Activity Scale; KOOS: Knee injury and Osteoarthritis Outcome Scale. |
Correlations between the K-SES and the determinants
All measures on Symptoms and Function Factors correlated significantly (rs = 0.3–0.5, p = 0.01) with K-SES except of the variable TegnerPre-injury, i.e. if the patients considered themselves to have resumed their pre-injury physical activity level. The correlation coefficients between the K-SES and the independent measures are presented in Table II. A significant correlation (rs = 0.3, p = 0.01) was also noted between K-SESABCD and a Personal Factor, the Internal Locus of Control. None of the factors of Previous Experience correlated significantly with the K-SESABCD, however.
| Table II. Correlation coefficients (Spearman’s r) for the K-SES and all the independent measures (IM 1–39). |
| | K-SES |
| | ABCD | ABC | D |
| Personal factors | | | |
| 1. Gender | 0.09 | 0.01 | 0.15 |
| 2. Surgery | 0.13 | 0.10 | 0.20* |
| 3. PASPresent | 0.21* | 0.19* | 0.27** |
| 4. TegnerPresent | 0.22* | 0.18* | 0.28** |
| 5. Age | –0.08 | 0.03 | –0.13 |
| SF-36 | | | |
| 6. Physical Functioning | 0.11 | 0.10 | 0.12 |
| 7. Role – Physical | 0.07 | 0.06 | 0.07 |
| 8. Bodily Pain | –0.12 | –0.15 | –0.09 |
| 9. General Health | –0.05 | –0.03 | 0.00 |
| 10. Vitality | 0.06 | 0.07 | 0.03 |
| 11. Social Functioning | 0.12 | 0.18 | 0.05 |
| 12. Role – Emotional | –0.08 | –0.08 | –0.04 |
| 13. Mental Health | 0.11 | 0.11 | 0.10 |
| CSQ | | | |
| 14. Diverting Attention | –0.01 | 0.03 | –0.05 |
| 15. Reinterpreting Pain | 0.08 | 0.08 | 0.10 |
| 16. Coping | 0.07 | 0.06 | 0.09 |
| 17. Ignoring | 0.22* | 0.19* | 0.22* |
| 18. Praying | –0.10 | –0.05 | –0.08 |
| 19. Catastrophizing | –0.03 | –0.01 | –0.03 |
| 20. In Behaviour | 0.05 | 0.08 | 0.04 |
| 21. Controlling Pain | 0.19* | 0.21* | 0.22* |
| 22. Decreasing Pain | 0.24* | 0.31** | 0.15 |
| MHLC | | | |
| 23. Internal Locus of Control | 0.31** | 0.32** | 0.30** |
| 24. External Locus of Control | –0.13 | –0.09 | –0.11 |
| 25. Locus of Control by Chance | –0.19* | –0.22* | –0.12 |
| Previous experience factors | | | |
| 26. InjuryPrevious | 0.01 | –0.07 | 0.03 |
| 27. IllnessPrevious | –0.05 | –0.03 | –0.06 |
| 28. InjuryExperience | 0.01 | 0.09 | –0.03 |
| 29. IllnessExperience | 0.02 | 0.00 | 0.04 |
| 30. PASPre-injury | –0.03 | –0.04 | 0.00 |
| 31. TegnerPre-injury | 0.11 | 0.05 | 0.15 |
| Symptom and function factors | | | |
| 33. PASResumed | 0.28** | 0.29** | 0.24** |
| 32. TegnerResumed | 0.12 | 0.14 | 0.13 |
| 34. KOOSSymptoms | 0.26** | 0.29** | 0.25** |
| 35. KOOSPain | 0.25** | 0.27** | 0.22* |
| 36. KOOSAdl | 0.30** | 0.29** | 0.29** |
| 37. KOOSSports/Recreation | 0.45** | 0.46** | 0.43** |
| 38. KOOSQoL | 0.39** | 0.39** | 0.38** |
| 39. Lysholm score | 0.51** | 0.52** | 0.50** |
| *Significant p < 0.05, **significant p < 0.01. MHLC: Multidimensional Health Locus of Control; CSQ: Coping Strategies Questionnaire; KOOS: Knee Injury and Osteoarthritis Outcome Score; K-SES: Knee Self-Efficacy Scale; PAS: Physical Activity Scale. |
Stepwise linear regression
The results of the stepwise linear regression analysis for the K-SES are presented in Table III. The most important determinant found in the present study was the Lysholm score for symptom and function, as well as the way the patients perceived their sports and recreational function. The most important Personal Factor for determining self-efficacy was Internal Locus of Control. A model using the Lysholm score, KOOSSport/Recreation, Internal Locus of Control and Locus of Control by Chance explained 40% of the variance in the complete K-SES. For self-efficacy right now (K-SESABC), a model of the Lysholm score, KOOSSport/Recreation, Internal Locus of Control and Locus of Control by Chance explained 41% of the variance. For future perceived self-efficacy (K-SESD), a model of the Lysholm score, KOOSSport/Recreation, TegnerPresent level and Internal Locus of Control explained 38% of the variance.
| Table III. Forward stepwise linear regression for the K-SES. |
| | Adj R2 | Beta | p-value |
| K-SESABCD | | | |
| Lysholm score | 0.258 | 0.348 | 0.000 |
| KOOSSports/Recreation | 0.345 | 0.305 | 0.000 |
| Internal Locus of Control | 0.374 | 0.181 | 0.018 |
| Locus of Control by Chance | 0.395 | –0.161 | 0.032 |
| K-SESABC | | | |
| Lysholm score | 0.270 | 0.350 | 0.000 |
| KOOSSports/Recreation | 0.357 | 0.304 | 0.000 |
| Internal Locus of Control | 0.389 | 0.186 | 0.014 |
| Locus of Control by Chance | 0.412 | –0.166 | 0.025 |
| K-SESD | | | |
| Lysholm Score | 0.265 | 0.265 | 0.000 |
| KOOSSports/Recreation | 0.332 | 0.290 | 0.001 |
| TegnerPresent | 0.360 | 0.167 | 0.032 |
| Internal Locus of Control | 0.377 | 0.155 | 0.047 |
| K-SESABCD without the Lysholm score | | | |
| KOOSSports/Recreation | 0.231 | 0.441 | 0.000 |
| Internal Locus of Control | 0.281 | 0.230 | 0.005 |
| Locus of Control by Chance | 0.300 | –0.158 | 0.049 |
| KOOS: Knee Injury and Osteoarthritis Outcome Score; K-SES: Knee Self-Efficacy Scale. |
To ensure that no other dimensions on the KOOS were excluded due to collinearity with the Lysholm score, an additional stepwise regression was performed without the Lysholm score. No additional dimensions on the KOOS were, however, included by the stepwise regression model. Excluding the Lysholm score from the model resulted in 30% of the variance in the complete K-SES being explained by KOOSSport/Recreation, together with Internal Locus of Control and Locus of Control by Chance.
Discussion
The main findings of this study were that about 40% of self- efficacy, as measured by the K-SES, was explained by self-reported symptoms and functions, as well as the patient’s locus of control. The determinants of self-efficacy in the rehabilitation of patients with an ACL injury are therefore dependent mostly on the way the patient interprets his/her knee symptoms and functions and the degree to which he/she believes that the outcome after injury or surgery is directly related to his/her individual behaviour.
The study population comprised typically active people with an ACL injury, ranging in physical activity level from 3 to 10 on the Tegner activity scale before the injury and from 1 to 10 at the 1-year follow-up. The means for the Lysholm score and the 5 dimensions on the KOOS were in accordance with other studies of patients with an ACL injury (20, 22). Considering the relatively young age (mean age 31.2 years) and mechanism of injury (during sports activity), it may not be surprising to find that perceived self-efficacy was relevant to the way the patients perceived their sports and recreational function.
In the present study, all the variables on Symptoms and Function correlated significantly with the K-SES, except if the patients considered themselves to have resumed their pre-injury physical activity level (TegnerPre-injury). One important determinant found in the present study was the Lysholm score, a score frequently used to assess patients with an ACL injury (23). The Lysholm score has also been found to be an important determinant of patient satisfaction with outcome after an ACL reconstruction (24). In our study, the KOOSSport/Recreation, together with the Lysholm score, explained about 33% of the variance in patients’ self-efficacy. The 8 items of the Lysholm score combine knee symptoms and functions into 1 score. The KOOS, a more comprehensive 5-dimensional score, has 42 items for symptoms and functions of the knee. Even though all 5 dimensions on the KOOS had similar correlations with patients’ self-efficacy, only the dimension of KOOSSport/Recreation added to our linear regression model for determining self-efficacy in patients with an ACL injury. Excluding the Lysholm score, for a test of collinearity, did not add to the results in this study. This means that the Lysholm score was more sensitive in the present study than the KOOS in reflecting knee symptoms and functions when determining self-efficacy in patients with an ACL injury.
In the present study, the most important Personal Factor for determining self-efficacy was Internal Locus of Control, indicating that patients with a high level of self-efficacy believe that their outcome after injury or surgery is related to a large degree to their individual behaviour. Furthermore, a significant negative correlation was also found between self-efficacy and Locus of Control by Chance, entering the linear regression model as a determinant of present self-efficacy (K-SESABC). This indicates that patients with a high level of self-efficacy believe that their outcome after injury or surgery is determined to a lesser degree by fate, luck or chance.
Personal Factors, such as age, gender and physical activity level, did not determine the degree of self-efficacy one year after injury/surgery. In a study of the determinants of patient satisfaction with outcome after ACL reconstruction surgery, returning to physical activity level, but not age and gender, was found to be associated with patient satisfaction (24).
In the present study, we also found that perceived future self-efficacy (K-SESD) correlated significantly with the choice of treatment, and whether to undergo surgery. This is interesting, as it has not yet been proven in any randomized, controlled study whether surgical intervention is necessary. Both surgical and non-surgical treatment have produced acceptable function, but also failures (25, 26). The importance of preparing the patient to understand the seriousness of the injury before initiating treatment such as surgery has been discussed in the literature (25, 27). It could therefore be hypothesized that it could be important to consider the patients’ degree of self-efficacy when deciding whether they should undergo surgery. However the choice of treatment did not enter as an important determinant for self-efficacy in our linear regression model.
None of the independent measures for coping with pain (CSQ) as well as for quality of life (SF-36) contributed to explain the determinants of self-efficacy. Coping with functional ability may be better correlated to perceived self- efficacy than coping with pain, but this subject requires further research. Furthermore, a follow-up period of one year after ACL injury/surgery may be too short a time to influence the patients’ quality of life.
Previous Experience did not determine self-efficacy in the present study. Past performance, vicarious experience, motivation, persuasion and negative feedback are sources of self-efficacy according to the cognitive theory (1). In spite of this, the correlation between factors of Previous Experience and the K-SES was low. Approximately 50% of the patients in this study had experience of multiple injuries. Psychological difficulties have been shown to be more frequent in the first-time injured compared with multiple-injury patients (28).
A limitation of the present study is that our recording of previous experience of injuries/illness is not comprehensive enough to identify any differences between the patients with earlier multiple injury/illness and the first-time injured. Nevertheless, it is important to consider the patients’ previous experience of injury/illness for self-efficacy, and further studies are needed. Another potential limitation is that the PAS has not been tested for reliability. Self-efficacy also appears to comprise other aspects of importance that have not been explored in the present study. We were able to detect approximately 40% of the determinants in our model for self-efficacy and there must thus be other factors that are important for self-efficacy. Such factors of importance could be the rehabilitation environment, as well as the experience and personal skills of doctors and therapists. These factors may be difficult to measure, but they may play an important role in rehabilitation in order to strengthen self-efficacy for physical tasks in patients with an ACL injury.
To summarize, the present study demonstrates that the K-SES was closely related to self-reported symptoms and functions, as well as to internal locus of control. The single most important determinant of self-efficacy in patients with an ACL injury was how the patient felt about his/her knee function in sports and recreation activities. Because of their relatively young age and the fact that the patients had been injured during sports activity, it appears that the patients’ perceived self-efficacy in terms of sports and recreational function is important. The other important determinant of self-efficacy in patients with an ACL injury was the internal locus of control, meaning that patients who have strong self-efficacy believe that their outcome after injury or surgery is directly related to their individual behaviour.
In addition, perceived self-efficacy of future capability appears to be influenced by the present physical activity level (TegnerPresent). The rehabilitation of a patient who is physically fit and determined to resume his/her prior activity may be more successful because of that patient’s strong self-efficacy. As a result, the strategies may have to be different when dealing with a patient who is less physically fit and has poorer self-efficacy.
This study has added to our knowledge of the potential role of self-efficacy in patients with an ACL injury. Further research is needed in order fully to understand self-efficacy and its role in rehabilitation.
Acknowledgements
This study was supported by a grant from the Swedish National Centre for Research in Sports and the Local Research and Development Council of Göteborg and southern Bohuslän.
References
1. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977; 84: 191–215.
2. Thomee P, Wahrborg P, Borjesson M, Thomee R, Eriksson BI, Karlsson J. Self-efficacy, symptoms and physical activity in patients with an anterior cruciate ligament injury: a prospective study. Scand J Med Sci Sports 2006 (Epub ahead of print)
3. Maly MR, Costigan PA, Olney SJ. Determinants of self-report outcome measures in people with knee osteoarthritis. Arch Phys Med Rehabil 2006; 87: 96–104.
4. Thomeé P, Wahrborg P, Borjesson M, Thomeé R, Eriksson BI, Karlsson J. A new instrument for measuring self-efficacy in patients with an anterior cruciate ligament injury. Scand J Med Sci Sports 2006; 16: 181–187.
5. Bandura A. Human agency in social cognitive theory. Am Psychol 1989; 44: 1175–1184.
6. Crossman J. Psychological rehabilitation from sports injuries. Sports Med 1997; 23: 333–339.
7. Johnson U. Coping strategies among long-term injured competitive athletes. A study of 81 men and women in team and individual sports. Scand J Med Sci Sports 1997; 7: 367–372.
8. Thomeé P, Thomeé R, Karlsson J. Patellofemoral pain syndrome: pain, coping strategies and degree of well-being. Scand J Med Sci Sports 2002; 12: 276–281.
9. Nyland J, Johnson DL, Caborn DN, Brindle T. Internal health status belief and lower perceived functional deficit are related among anterior cruciate ligament-deficient patients. Arthroscopy 2002; 18: 515–518.
10. Beckham JC, Burker EJ, Rice JR, Talton SL. Patient predictors of caregiver burden, optimism, and pessimism in rheumatoid arthritis. Behav Med 1995; 20: 171–178.
11. Soderlund A, Olerud C, Lindberg P. Acute whiplash-associated disorders (WAD): the effects of early mobilization and prognostic factors in long-term symptomatology. Clin Rehabil 2000; 14: 457–467.
12. Kyhlback M, Thierfelder T, Soderlund A. Prognostic factors in whiplash-associated disorders. Int J Rehabil Res 2002; 25: 181–187.
13. Sullivan M, Karlsson J, JE W, editors. SF-36 Swedish manual and interpretation guide. Göteborg: Health Care Research Unit, Medical Faculty, Sahlgrens Hospital; 1994.
14. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 1985; 198: 43–49.
15. Saltin B, Grimby G. Physilogical analysis of middle-aged and former athletes. Circulation 1968; 38: 1104–1105.
16. Ware JE Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992; 30: 473–483.
17. Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain 1983; 17: 33–44.
18. Wallston KA, Wallston BS, DeVellis R. Development of the Multidimensional Health Locus of Control (MHLC) Scales. Health Educ Monogr 1978; 6: 160–170.
19. Jensen. L. Coping stratergies questionnaire (CSQ): reliability of the Swedish version of the CSQ. Scand J Behav Ther 1993; 22: 139–145.
20. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS) – development of a self-administered outcome measure. J Orthop Sports Phys Ther 1998; 28: 88–96.
21. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 1982; 10: 150–154.
22. Dedmond BT, Almekinders LC. Operative versus nonoperative treatment of knee dislocations: a meta-analysis. Am J Knee Surg 2001; 14: 33–38.
23. Suk M, Hanson B, Norvell D, D. H. AO Handbook, musculoskeletal outcomes measures and instruments. Stuttgart and New York: Thieme; 2005.
24. Kocher MS, Steadman JR, Briggs K, Zurakowski D, Sterett WI, Hawkins RJ. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. J Bone Joint Surg Am 2002; 84-A: 1560–1572.
25. Almekinders LC, Dedmond BT. Outcomes of the operatively treated knee dislocation. Clin Sports Med 2000; 19(3): 503–518.
26. Casteleyn PP, Handelberg F. Non-operative management of anterior cruciate ligament injuries in the general population. J Bone Joint Surg Br 1996; 78: 446–451.
27. Maddison R, Prapavessis H, Clatworthy M. Modeling and rehabilitation following anterior cruciate ligament reconstruction. Ann Behav Med 2006; 31: 89–98.
28. Johnson U. The multiply injured versus the first-time-injured athlete during rehabilitation: a comparison of nonphysical characteristics. J Sport Rehabil 1996; 5: 293–304.