As with eye movements in locked-in syndrome, severe motor dysfunction should be coped with by an agreed system of interpretation to express feelings and needs. However, it is possible that such patients might make errors in the agreed system of interpretation through fatigue, which would cause misunderstandings. We report here a new questioning and verifying strategy for an agreed system of interpretation. Our questioning strategy is characterized by repeating questions in different forms, specifically by affirmative and negative sentences (Double-Checked agreed system of interpretation). When the patient wants to express “Yes”, a single movement is required for an affirmative question and no movement is required for a negative one. When the patient wants to express “No”, no movement is required for an affirmative question and one movement is required for a negative one. The Double-Checked agreed system of interpretation can help patients to cope with fatigability and can also help to prevent misunderstandings. If the same responses to both affirmative and negative questions are given, we can consider that those answers reflect fatigue. In addition, we have developed a strategy to evaluate the patient’s understanding of the Double-Checked agreed system of interpretation by modifying the Western Aphasia Battery. This report describes how to apply the Double-Checked agreed system of interpretation, using the example of a 48-year-old brain-injured man with minimal motor function and severe fatigability.
Key words: motor dysfunction, neuropsychological impairment, communication disorder, locked-in syndrome, quality of life.
J Rehabil Med 2007; 39: 185–188
Correspondence address: Keiji Hashimoto, Department of Rehabilitation Medicine, The Jikei University School of Medicine, 3-25-8, Nishi-Shinbashi, Minato-ku,Tokyo, 105-8461, Japan. E-mail: keiman@jikei.ac.jp
Submitted July 12, 2006; accepted October 18, 2006.
Introduction
Quadriplegia and anarthria (1, 2) are among the most severe conditions that reduce communication skills of patients. Various diseases or injuries can cause these severe outcomes. These include stroke, traumatic brain injury, encephalitis, amyotrophic lateral sclerosis, and other neuronal diseases, i.e. conditions that can extensively damage bilateral corticobulbur and corticospinal tracts (3–9).
As with eye movements in locked-in syndrome (10), these patients should be provided with a reliable agreed system of interpretation (ASI) (1) to express feelings and needs. Generally, 2 movements signify “Yes” and 1 movement signifies “No” (general ASI; G-ASI). However, mistakes may occur when such patients become tired, as patients may be able to move their body only once in spite of the intention to express “Yes”. The risk is higher in patients with decreased alertness. Thus, when such patients have complication-related neuropsychological impairment, an appropriate questioning and verifying strategy should be developed for medical staff and carers (1).
We report here a new questioning and verifying strategy for ASI to cope with fatigability. The questioning strategy is characterized by repeating questions in different forms, specifically by affirmative and negative sentences (Double-Checked ASI; DC-ASI). When the patient expresses “Yes”, a single movement is required to answer an affirmative question and no movement is required for a negative question. When the patient expresses “No”, no movement is required to answer an affirmative question and a single movement is required for a negative question. DC-ASI can help to cope with fatigability in such patients and can also help to prevent our misunderstanding of the patient’s wishes. If there is no movement in response to both an affirmative and negative question, it can be concluded that the answer reflects fatigue. This report describes the development and application of the DC-ASI for a 48-year-old brain-injured man with minimal motor function and decreased alertness.
Case Report
Subject
A 48-year-old man was admitted to hospital because of sudden gait disturbance. He had had diabetes mellitus and hypertension, and also had had 2 episodes of cerebral infarction. He had had mild right hemiparesis as a sequela prior to the current admission.
On the date of admission, neurological examination revealed mild right hemiparesis and mild dysarthria. Magnetic resonance imaging (MRI) showed new cerebral infarctions in the left internal capsule, right putamen and right corona radiata. Conservative therapy was administered. On the 5th hospital day, weakness of the left upper limb became evident. On the 8th hospital day, coma and decorticate rigidity developed and persisted. MRI showed multiple new lesions. From the 43rd hospital day, decorticate rigidity gradually improved and the patient’s eyes were open.
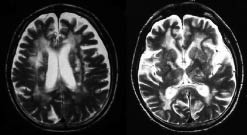
On the 60th hospital day, we noted minimal movements, examples of which are blinking, visual pursuit, and right arm movement. Neurological examination showed quadriplegia and anarthria (1, 2) with preservation of consciousness. His motor function was minimal and he was totally dependent with regard to activities of daily living. MRI showed multiple cerebral infarctions in bilateral basal ganglia and subcortex (Fig. 1), with no brain-stem insult. Electroencephalography showed a slow alpha pattern with mild non-specific slow activity. At that time, development of an ASI was required (1) because the patient had lost all skills of expression.
Fig. 1. Magnetic resonance imaging showing multiple cerebral infarctions in bilateral basal ganglia and diffuse subcortex.
Developing a general ASI
Minimal movements of the lips, left foot, right thumb, right hand and right arm were noted. Blinking and visual pursuit were evident. Neurological examination showed that the blinking and lip movement could not be distinguished from normal reflexes. Also, this examination revealed that movement of the left foot, right thumb and right hand could not be distinguished from involuntary movements. Visual pursuit was seen often, but could not be performed in response to instructions. Right arm movement could most frequently be performed in response to instructions. We provided the patient with the information that “Yes” would be signified by moving his right arm and “No” would be signified by no movement in that arm as a G-ASI. However, it was observed that the movement had a tendency to decrease gradually as it was repeated. In addition, spasticity had a tendency to increase gradually as the movement was repeated, and this caused involuntary movement. These observations suggested physical and mental fatigue. Such a patient might make a mistake in the G-ASI due to fatigue. Thus, we could not apply the G-ASI to this patient. Therefore, a DC-ASI was considered necessary to cope with the patient’s fatigue and to prevent our misunderstanding of his wishes.
MethodS
Developing a Double-Checked ASI
A new questioning strategy was devised, whereby we asked the patient a question twice by using both an affirmative and negative question. When the patient wanted to express “Yes”, a single movement was required for an affirmative question and no movement was required for a negative question. When the patient wanted to express “No”, no movement was required for an affirmative question and a single movement was required for a negative question. In addition, a verification strategy for medical staff and carers was developed. Specifically, if there was no movement in response to an affirmative question and no movement in response to a negative question (no response; NR) or movement for an affirmative question and movement for a negative question (equivocal response; ER), we decided to consider the answers to be a reflection of fatigue and to give the patient sufficient rest.
Evaluating his understanding of DC-ASI strategy
We modified the subscale of the Western Aphasia Battery (WAB) Japanese version (11, 12) Section II; Auditory Verbal Comprehension. In this section answers should be either “Yes” or “No”. We modified the original questions into affirmative and negative sentences. We asked the patient these modified questions by the DC-ASI.
Results
Table I shows the same sentence that was constructed both affirmatively and negatively, with the patient’s answers to both affirmative and negative questions. The table shows whether the meaning of the answer was “Yes”, “No”, “NR” or “ER” and whether his answer was “correct”, “wrong” or “not detectable”.
| Table I. Modified questions from Western Aphasia Battery Japanese version |
| Question | Affirmative questions (AQ) (negative questions (NQ)) | Patient’s response to AQ | Patient’s response to NQ | Meaning of patient’s answer | Correct or wrong |
| 1 | Your name is (not) Mr Sakai? | None | One | No | Correct |
| 2 | Your name is (not) Mr Nakagawa? | None | One | No | Correct |
| 3 | Your name is (not) ”real name of patient”? | One | None | Yes | Correct |
| 4 | You (don’t) live in Kumamoto? | One | One | ER | ND |
| 5 | You (don’t) live in ”real residence of patient”? | One | None | Yes | Correct |
| 6 | You (don’t) live in Aomori? | One | One | ER | ND |
| 7 | You are (not) a man? | One | None | Yes | Correct |
| 8 | You are (not) a doctor? | None | One | No | Correct |
| 9 | I am (not) a man? | One | None | Yes | Correct |
| 10 | The lights are (not) on in this room? | None | One | No | Correct |
| 11 | The door is (not) closed? | One | None | Yes | Correct |
| 12 | This is (not) a hotel? | None | None | NR | ND |
| 13 | This is (not) a ”real test location”? | One | One | ER | ND |
| 14 | You are (not) wearing red pyjamas? | None | One | No | Correct |
| 15 | Paper will (not) burn in fire? | One | One | ER | ND |
| 16 | March (doesn’t) come before June? | One | None | Yes | Correct |
| 17 | You (don’t) eat a banana before you peel it? | None | One | No | Correct |
| 18 | It (doesn’t) snow in July? | None | One | No | Correct |
| 19 | A horse is (not) larger than a dog? | One | None | Yes | Correct |
| 20 | You (don’t) cut the grass with an axe? | None | One | No | Correct |
| If a single movement (One) of his right arm to affirmative question (AQ) and no movement (None) to negative question (NQ) were observed, the meaning was regarded as “Yes”. Similarly, if “None” to AQ and “One” to NQ were observed, the meaning was regarded as “No”. “Yes” and “No” were ensured whether the patient’s meaning was “correct” or “wrong”. On the other hand, an answer of “None” to AQ and “None” to NQ was considered as no response (NR), and “One” to AQ and “One” to NQ was considered as an equivocal response (ER). When NR or ER was observed, we could not determine the patient’s meaning and considered this as “not detectable (ND)”. For example, in question 7, we asked “You are a man?” and the answer was “One”. Then we asked “You are not a man?” and the answer was “None”. The meaning was regarded as “Yes”. The patient’s meaning was correctly matched to the fact and considered “correct”. |
One cycle of this evaluation by DC-ASI was repeated 6 times to ascertain its reliability (Table II). We could detect “Yes” or “No” in 78.3% (93/120) of the answers. Of the 93 answers, 92 were “correct” (98.9%). This indicated that not only did the patient understand the DC-ASI strategy, but also that his cognitive function was sufficient for simple conversation.
| Table II. Evaluation of the Double-Checked agreed system of interpretation (DC-ASI). Results of 6 trials |
| | DC-ASI |
| Question | Trial 1 | Trial 2 | Trial 3 | Trial 4 | Trial 5 | Trial 6 |
| 1 | C | C | C | ND | C | C |
| 2 | C | C | ND | C | C | C |
| 3 | C | C | C | ND | C | C |
| 4 | ND | C | C | C | C | ND |
| 5 | C | C | C | ND | C | C |
| 6 | ND | C | C | ND | C | ND |
| 7 | C | C | W | C | ND | C |
| 8 | C | C | ND | C | ND | ND |
| 9 | C | C | C | C | C | C |
| 10 | C | C | ND | ND | C | C |
| 11 | C | C | C | C | C | C |
| 12 | ND | C | C | C | C | C |
| 13 | ND | C | C | ND | C | C |
| 14 | C | C | C | C | C | ND |
| 15 | ND | C | ND | ND | C | C |
| 16 | C | ND | C | C | ND | C |
| 17 | C | C | C | C | C | C |
| 18 | C | ND | C | C | C | C |
| 19 | C | C | C | ND | C | C |
| 20 | C | C | C | C | C | C |
| ”Yes” or ”No” answers were used to determine whether the meaning was ”correct (C)” or ”wrong (W)”. On the other hand, answers that were regarded as ”no response” or “equivocal response” were considered as “not detectable (ND)”. |
After introduction of DC-ASI
The DC-ASI provided the patient with more opportunity to obtain appropriate support and the environment that he desired. Family members understood that his cognitive function was good enough for simple communication. Consequently, his family could communicate with him more confidently using various aids, including pictures. We could successfully introduce him to another hospital specialized in chronic-stage rehabilitation.
Discussion
In this case, the patient’s brain had been severely damaged by multiple cerebral infarctions. He emerged from coma in a state of quadriplegia and anarthria with preservation of consciousness after a several-week-decorticated state. He had lost almost all motor function. He had severely impaired communicative and interactive capacities. He was in a low responsive state. His neurological state was similar to that of locked-in syndrome (1–3), however, his clinical course, several-week-decorticated state, suggested minimal responsive state after vegetative state. In addition, since his vertical eye movement was not available for communication, we had to develop an original communication strategy. In evaluating his minimal movements, we found that he could perform visual pursuit at almost full range, but that his eye movements could not be made in response to our instructions. It made us suspect the presence of apraxia or other neuropsychological impairments. In fact, sometimes he could not obey very simple instructions, and appropriate responses tended to decrease gradually. This suggested that neuropsychological impairment that included, for example, decreased alertness and attention disturbance, might be present, causing mental fatigability, alongside the physical fatigability caused by his physical impairment. His clinical course also made us suspect that these conditions caused his low responsive state simultaneously. Our intervention was developed to reduce the degree of effort required for communication by the patient to cope with these conditions.
To apply the DC-ASI to such patients, cognitive function should be sufficient for simple conversation. Therefore, their understanding of the DC-ASI strategy needed to be ascertained by using a modified WAB. Thus, the DC-ASI cannot be applied to patients with severe cognitive dysfunction. However, severe motor dysfunction and mild cognitive dysfunction are often seen in patients with severe brain damage. Although our intervention is not suitable for application in all patients with brain injuries, it can be used in many brain injuries. To develop an appropriate method of selecting patients, it is of crucial importance to validate our intervention by other previous evaluations.
Other communication approaches would support his efforts at communication, for example, pictures, written words or signs, and aided scanning techniques, whereby another person points and the patient reacts to, for example, the intended line or picture. However, it is possible that any aided scanning technique could cause misunderstanding by those around the patient, as with the ASI. We must emphasize that no technique should be applied until it is ascertained that the patient understands the communication strategy. Very basic communication techniques can be useful in ascertaining a patient’s understanding. “Yes-No communication” is considered to be most basic technique. DC-ASI can be applied for ascertaining the patient’s understanding about a more effective communication strategy. Although our intervention could not provide the patient with skills to express his thoughts, it did allow him the opportunity for further rehabilitation in relation to communication.
We consider that this intervention could help to provide increased opportunities for social integration to patients with physical fatigability due to severe motor dysfunction and also with mental fatigability caused by decreased alertness, etc. To cope with the patient’s fatigue and to prevent our misunderstand- ing of his wishes, an appropriate communication strategy that includes providing sufficient rest and evaluates the tendency to make movement mistakes would play an important role.
REFERENCES
1. Smith E, Delargy M. Locked-in syndrome. BMJ 2005; 330: 406–409.
2. Richard I, Pereon Y, Guiheneu P, Nogues B, Perrouin-Verbe B, Mathe JF. Persistence of distal motor control in the locked-in syndrome. Review of 11 patients. Paraplegia 1995; 33: 640–646.
3. Haig AJ, Katz RT, Sahgal V. Mortality and complications of the locked-in syndrome. Arch Phys Med Rehabil 1987; 68: 24–27.
4. Katz RT, Haig AJ, Clark BB, Di Paolo RJ. Long-term survival, prognosis and life-care planning for 29 patients with chronic locked-in syndrome. Arch Phys Med Rehabil 1992; 73: 403–408.
5. Leon-Carrion J, van Eeckhout P, Dominguez-Morales Mdel R, Perez Santamaria FJ. The locked-in syndrome: a syndrome looking for a therapy. Brain Inj 2002; 16: 571–582
6. Hayashi H, Oppenheimer EA. ALS patients on TPPV. Totally locked-in state, neurologic findings and ethical implications. Neurology 2003; 61: 135–137.
7. Khurana RK, Genut AA, Yannakis GD. Locked-in syndrome with recovery. Ann Neurol 1980; 8: 439–441.
8. Patterson JR, Grabois M. Locked-in syndrome: a review of 139 cases. Stroke 1986; 17: 758–764.
9. Doble JE, Haig AJ, Anderson C, Katz R. Impairment, activity, participation, life satisfaction and survival in persons with locked-in syndrome for over a decade. J Head Trauma Rehabil 2003; 5: 435–444.
10. Bauer G, Gerstenbrand F, Rumpl E. Varieties of locked-in syndrome. J Neurol 1979; 221: 77–91.
11. Sugishita M, editor. The Western Aphasia Battery Japanese version. Tokyo: Igaku-Shoin; 1986.
12. Kertesz A, editor. The Western Aphasia Battery. New York: Grune and Stratton, Inc.; 1982.