Joanna L. Walker1, Lisa M. Cohen2 and George Kroumpouzos1
1Department of Dermatology, The Warren Alpert Medical School of Brown University, 593 Eddy St, Providence, RI 02903, and 2Strata Dx, Lexington, Massachusetts, USA. E-mail: gk@gkderm.com
Accepted Nov 12, 2014; Epub ahead of print Nov 14, 2014
Leukemia cutis is an uncommon manifestation of chronic lymphocytic leukemia (CLL); a large study of 751 CLL patients identified leukemia cutis in only 3 cases (0.3%) (1). Lesions of leukemia cutis tend to occur late in the disease with nonspecific, isolated or grouped erythematous or violaceous papulonodules and/or plaques that are typically located on the head and neck. The lesions may mimic other conditions such as granulomatous rosacea or rhinophyma when localized on the central face or present on the bilateral helices and/or earlobes (2). Herein we present the first case of bilateral auricular involvement treated successfully with involved field electron beam therapy.
CASE REPORT
A 39-year-old Caucasian man presented to dermatology with a two-year history of lumps on the bilateral earlobes. The lesions fluctuated in size, at times growing larger and becoming very painful. There was no ulceration or bleeding from the lesions, no other skin problems, and no associated factors. The review of systems was negative, and the patient had no history of medical problems. Examination revealed dusky red soft nodules on the earlobes and erythematous papulonodules on the bilateral helices and tragus of the right ear (Fig. 1a). There were no other skin findings, and no palpable lymphadenopathy.
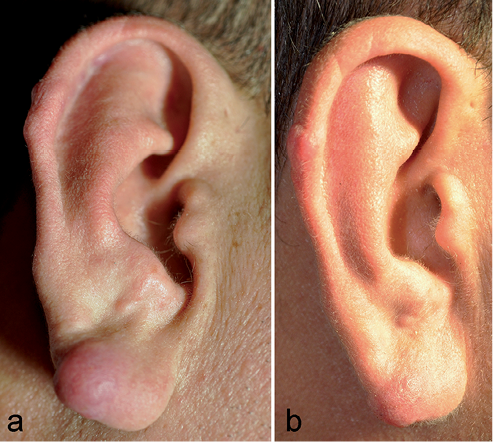
An excisional skin biopsy showed a nodular superficial and deep dermal infiltrate of small atypical lymphocytes and a Grenz zone (Fig. 2a, b). Immunoperoxidase studies highlighted B lymphocytes co-expressing CD20, CD5, CD23 and Bcl-2, and comprising 90% of the infiltrate (Fig. 2c, d). Bcl-6 was modestly positive. The lymphocytes were CD10–, and the majority did not express immunoglobulin kappa or lambda light chain by in situ hybridization. CD3 and CD5 stains highlighted abundant background T cells with a CD4:8 ratio of 3:1. Gene rearrangement studies showed clonal B- and T-cell populations. A pathologic diagnosis of cutaneous involvement by CLL was made. Subsequent workup showed a normal white blood cell count with a lymphocyte predominance of 5.98 × 109l–1 or 56.8% (normal 1.00–4.00 × 109l–1; 15–50%). Flow cytometry studies showed clonal B lymphocytes that co-expressed CD5, CD23 and weak surface lambda light chain, comprising 48% of lymphocytes. Thoracic and abdominal/pelvic computed tomographic scans were negative. These findings confirmed the diagnosis of CLL. Small lymphocytic lymphoma was ruled out by the absence of lymphadenopathy and splenomegaly. Our patient was treated with involved field electron beam therapy. A total energy dose of 4 Gy (to convert to rad, multiply by 100) was delivered in two fractions over one elapsed day to each ear. The auricular lesions decreased in number and size, and the swelling and pain resolved (Fig. 1b). Over a 5-month period following treatment, there has been no relapse.

Fig. 2. (a) Dense mononuclear cell infiltrate throughout the dermis and extending into the subcutaneous tissue, with a Grenz zone separating the infiltrate from the overlying epidermis. There is hemorrhage within the dermis and small cystic lesions in the upper dermis (hematoxylin-eosin, original magnification × 40); (b) higher magnification demonstrates a monotonous population of lymphoid cells in a sheet-like pattern with mild nuclear atypia and scant cytoplasm (hematoxylin-eosin, original magnification × 400); (c, d) CD5 (c) and CD20 (d) immunostains highlight the infiltrate strongly and diffusely (original magnification × 400).
DISCUSSION
The differential diagnosis of bilateral auricular lesions includes infectious (leprosy, leishmaniasis, tuberculosis), neoplastic (primary lymphoma, lymphocytoma cutis, Rosai-Dorfman disease, multicentric reticulohistiocytosis), and miscellaneous (sarcoidosis, perniosis, relapsing polychondritis, auricular pseudocyst, trauma/hematoma) skin disease (2). Cutaneous lesions in CLL localized exclusively to the bilateral ears have been only exceptionally reported (2–6). Leukemia cutis on the ears usually occurs in older patients with known or late-stage CLL, but as seen in our case, it can be the heralding feature in a young patient with otherwise subclinical disease.
The presence of leukemia cutis does not infer a worse outcome in CLL, and some authors reported an improved prognosis (3). Therefore, CLL leukemia cutis may be treated with local rather than systemic therapy, such as irradiation, excision, or intralesional steroids. Several focused treatment modalities have been used to control cutaneous disease in CLL including radiation therapy (7), ultraviolet light B (8), psoralen with ultraviolet A (PUVA) (8), and electrochemotherapy with bleomycin (9). A review of full body electron beam therapy for refractory cutaneous lymphoma and leukemia that included one case of CLL showed excellent palliative results in 92% of cases. Side effects of total body electron beam therapy are reportedly manageable and dose-related (10). Morbidity burden of localized treatment is lower but depends on the site treated. Low-dose involved field radiotherapy is an option for localized cutaneous lymphoma or in the situation of localized recurrence after total body electron beam therapy, with the option of re-irradiation at progression (10).
Our case adds to a few cases describing bilateral auricular involvement as a characteristic finding in CLL, and illustrates that it can be a warning sign of the disease. Dermatologists should be aware of this presentation, and consider CLL in the differential diagnosis of bilateral auricular lesions. To our knowledge, the present case is the first in which bilateral auricular involvement was treated successfully with involved field electron beam therapy.
The authors declare no conflict of interest.
REFERENCES
