Purulent Discharge from the Nipples: A Quiz
Elena del Alcázar Viladomiu, Anna Tuneu Valls, Maria Asunción Arregui Murua, Ane Jaka Moreno and Nerea Ormaeche- Pérez
Department of Dermatology, Hospital Universitario Donostia, Paseo Dr.Begiristain 107-116, Edificio Amara 2ªplanta, ES-20014 Donostia-San Sebastián, (Gipuzkoa), Spain. E-mail: elenadelalcazarviladomiu@gmail.com
A 21-year-old woman, smoking 7 cigarettes per day, was seen in our department because of lesions in both breasts. She described episodes of purulent drainage from her left nipple and periareolar area for the last 2 years. Lesions in the right areola began 6 months ago. She did not describe fever or physical discomfort. The patient had no history of hidradenitis, cystic acne or trauma to the nipple. She had no past pregnancies.
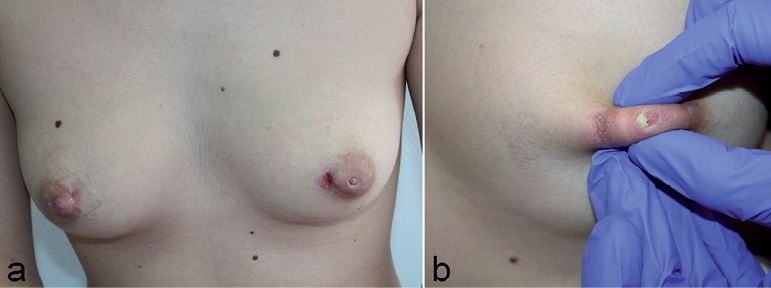
Cutaneous examination showed inverted nipple in the left breast with an ulcerated lesion in the areola’s internal border (Fig. 1a). Purulent material drained both from the nipple and the periareolar lesion upon lateral pressure (Fig. 1b). The right breast presented a little scar in the areola’s internal border.
doi: 10.2340/00015555-1745
Fig. 1. Inverted nipple of the left breast with an ulcerated lesion in the areola’s internal border. On the right breast, a scar without inflammatory signs in the areola’s internal border (a). Periareolar abscess and fistula. Purulent drainage from left nipple when it was pressed and it also shows an ulcerated lesion on the areola’s internal border (b).
Bacterial culture was negative and breast ultrasound proved normal.
What is your diagnosis? See next page for answer.
Purulent Discharge from the Nipples: A Comment
Acta Derm Venereol
Diagnosis: Zuska’s disease
Zuska’s disease (ZD) is a squamous metaplasia of lactiferous ducts, resulting in obstruction, ductal dilatation, and ductal inflammation (1). Zuska was the first to describe this disease in 1951 (2). Subsequently, different authors proposed other medical terms such as mammillary fistula, periductal mastitis or periareolar abscess, among others.
ZD usually affects young women of childbearing age, except during pregnancy and breastfeeding (3), with a mean age of 35 years. Its incidence is variable, usually ranging between 1–10%, depending on the studies reported (3). Cigarette smoking is the most important risk factor for development and severity of the metaplasia (1, 3, 4).
Histologically there is replacement of the normal double layer cuboid epithelium of the lactiferous ducts by flat epidermal epithelium (squamous metaplasia) (1).
Clinical features vary depending on the stage (1): ductal ectasia, suppurative galactophoritis, periareolar abscess and periareolar fistula.
Ductal ectasia, a pathologic dilatation of lactiferous ducts, stays asymptomatic in 30% of cases. Suppurative galactophoritis is characterised by peri- or subareolar sporadic and recurrent breast pain. Subareolar abscess causes local inflammatory signs and may be accompanied by fever and physical discomfort. The last stage is a periareolar fistula, which is a communication between a subareolar duct and the skin and is almost always associated with an inverted nipple.
The purulent drainage is not sterile; both aerobic and anaerobic organisms are isolated from abscesses in a high proportion of patients (5).
Antibiotics are the main treatment for duct ectasia and galactophoritis, but surgery is the only curative treatment for periareolar fistula (6). In the early stages, the abscess can be treated with oral antibiotics, and should be drained when it is fluctuant (6). Finally, smoking cessation is an important component of therapy.
Our patient was referred to the Gynaecology department for surgical excision. Pathology showed a periareolar abscess with many polymorphonuclear and lymphoplasmacytic cells, without malignant cells (Fig. 2).
Currently, she is being followed up and remains asymptomatic 9 months after surgery.
Fig. 2. Periareolar abscess. This histopathological image shows a periareolar infiltrate with many polymorphonuclear and lymphoplasmacytic cells corresponding to an inflammatory injury, without malignant cell (H&E × 20).

Despite the frequent cutaneous involvement in this disease there are few reports in the dermatological literature. We present this case because it is a rare disorder, and awareness of the condition facilitates correct diagnosis and treatment.
Acknowledgement
Marta Rezola Bajineta, Hospital Universitario Donostia, is acknowledged for the pathology photo.
References
