Johanna Mandelin, Anita Remitz, Hannele Virtanen and Sakari Reitamo
Skin and Allergy Hospital, Department of Dermatology, Helsinki University Central Hospital, Helsinki, Finland
Johanna Mandelin, Anita Remitz, Hannele Virtanen and Sakari Reitamo
Skin and Allergy Hospital, Department of Dermatology, Helsinki University Central Hospital, Helsinki, Finland
A one-year, randomized, double-blind study was conducted in 80 patients with atopic dermatitis treated with tacrolimus ointment or a corticosteroid regimen (hydrocortisone acetate 1% ointment for head and neck, hydrocortisone butyrate 0.1% ointment for trunk and limbs) to compare efficacy and safety, and effects on Th2-reactivity. The study was completed by 36/40 patients in the tacrolimus group, and 31/40 patients in the corticosteroid group. In both groups affected body surface area, eczema area and severity index, and transepidermal water loss decreased at months 6 and 12. Tacrolimus was superior for all efficacy scores at month 6, and in the head and neck area at month 12. Recall antigen reactivity increased at month 12 in both groups. Adverse events were reported by 40/40 patients in the tacrolimus, and by 34/40 patients in the corticosteroid group. Long-term treatment with topical tacrolimus or a corticosteroid regimen improves atopic dermatitis and recall antigen reactivity, suggesting an improvement in the Th1/Th2-balance. Key words: atopic dermatitis; hydrocortisone butyrate; randomized controlled trial; recall antigen; tacrolimus ointment.
(Accepted October 26, 2009.)
Acta Derm Venereol 2010; 90: 170–174.
Johanna Mandelin, Department of Dermatology, Skin and Allergy Hospital, Helsinki University Central Hospital, Meilahdentie 2, FIN-00250 Helsinki, Finland. E-mail: johanna.mandelin@hus.fi
Atopic dermatitis (AD) is an inflammatory skin condition that shows signs of decreased T-helper type 1 (Th1) and increased T-helper type 2 (Th2) immune reactivity. In patients with active AD this increases susceptibility to microbial infections of the skin, and increases serum levels of immunoglobulin E (S-IgE) (1). The decreased Th1 reactivity can be demonstrated as impaired reactions in skin tests with recall antigens (2), which indirectly measure delayed-type hypersensitivity. Patients receiving systemic immunosuppressive treatment also have impaired reactions (3), and are known to have increased susceptibility to infections and skin cancer (4, 5). We have previously observed an improvement in recall antigen reactions in an uncontrolled safety study with 48 adult AD patients treated for one-year with topical tacrolimus (6). To our knowledge there are no published studies on recall antigen reactions in patients with AD treated with topical corticosteroids.
Tacrolimus inhibits early gene transcription and activation of T cells. Topical tacrolimus (0.03% and 0.1% ointment) is indicated for the treatment of moderate-to-severe AD, and efficacy has been demonstrated in adults and children (7, 8). Long-term safety of tacrolimus ointment has been investigated in trials of up to 4 years duration (9, 10), and no increase in skin infections, skin cancer, or lymphomas has been detected (11–14).
Topical corticosteroids have long been the first-line treatment for AD, but their use is limited by the wide distribution of steroid-responsive elements in various cells and tissues. Prolonged use can lead to signs of skin atrophy, such as striae, and telangiectasias, and even to systemic side-effects, including growth-restriction in children, and glaucoma. Topical corticosteroids are approved only for short-term use, and there are, to our knowledge, only a few published long-term (12 months) studies on treatment with topical corticosteroids in AD (15, 16).
To further investigate and compare the long-term efficacy and safety of 0.1% tacrolimus ointment and a corticosteroid regimen, we performed a randomized, double-blind, comparative study in patients with AD.
PATIENTS AND METHODS
Study design
A one-year, randomized, double-blind, comparative study of tacrolimus ointment vs. a corticosteroid regimen was conducted in a single centre in Helsinki, Finland. The study was approved by the local ethics committee, and all patients gave written informed consent. Some of the efficacy and safety data from this study were included in a published 6-month clinical study that included 972 patients from 57 centres (17).
Patients and methods
Adults (aged ≥ 18 years) with moderate-to-severe AD according to the Rajka & Langeland criteria (18) were randomized 1:1 to treatment with 0.1% tacrolimus ointment (all affected body areas), or hydrocortisone acetate 1% ointment (head and neck) plus hydrocortisone butyrate 0.1% ointment (trunk and extremities). The ointment tubes were marked for treatment of either head and neck or trunk and limbs, and were identical in appearance in both groups. They were given to the patient and returned to the investigator in sealed boxes, and thus the investigator could not assess the ointment bases. AD flares were treated twice-daily until 7 days after clearance, and treatment resumed in the event of a recurrence or new flare. There was no limitation of ointment usage over 12 months. In the initial 6 months, assessments were made every month, and then at months 9 and 12. Prohibited therapies during the study included topical and systemic corticosteroids for the treatment of AD, topical and systemic antimicrobials influencing efficacy assessments, systemic antihistamines, coal tar, ultraviolet radiation treatments, hypnotics and sedatives, and systemic immunosuppressive agents. Patients were advised to minimize the exposure of treated areas to sunlight.
The primary end-point was response rate after 3 months of treatment, defined as the proportion of patients with ≥ 60% improvement in modified Eczema Area and Severity Index (mEASI) score, which we regarded as clinically significant improvement. Key end-points included clinical efficacy and safety, transepidermal water loss (TEWL), recall antigen testing, and S-IgE.
Assessments
Efficacy measures in the study included affected body surface area (BSA), and the Eczema Area and Severity Index (EASI) and mEASI scores. The mEASI is similar to the EASI, but includes an additional assessment of itch. From the EASI score we separately analysed the score for the head and neck area (eczema score for head and neck). Physician’s and patient’s assessment of global response, the response for the head and neck area, and adverse events were recorded throughout the study.
TEWL was measured at baseline and months 3, 6, 9 and 12, in nine target regions (three on the upper limbs, two each on the head and trunk, and one on the neck and lower limbs). Measurements were made with an Evaporimeter EP1 (servoMed, Stockholm, Sweden) according to published guidelines (19).
Recall antigen testing was carried out using the Multitest CMI (Institute Mérieux, Lyon, France) at baseline, and months 6 and 12. An eight-pronged applicator was used, containing seven antigens (tetanus, diphtheria, Streptococcus group C, tuberculin, Candida albicans, Trichophyton and Proteus) and one vehicle control (glycerol). Results were recorded as the Merieux score, which is the sum of the average diameters from positive reactions (induration at application site of ≥ 2 mm in diameter), and number of positive reactions.
S-IgE samples were collected at baseline, month 6 and month 12, and were measured by a fluorescence enzyme immunoassay (FEIA, CAP system; Pharmacia Diagnostics AB, Uppsala, Sweden).
Statistical analysis
Statistical analyses were performed with the statistical software package SPSS 13.0 for windows (SPSS Inc, Chicago, IL, USA). An intention-to-treat analysis was carried out for all data, using the last observation carried forward where appropriate. Changes in the variables before and after were tested with the Wilcoxon test; groups were compared using the Mann-Whitney test. Fisher’s exact test was used to compare the incidence of adverse events between the two treatment groups. Correlations between parameters were investigated using the Spearman test. A p-value of less than 0.05 was considered to be statistically significant.
RESULTS
Patients
The analyses included 80 patients (40 in each of the tacrolimus ointment and corticosteroid regimen groups). Baseline characteristics were well balanced between the two arms (Table I). The full 12-month study was completed by 36 patients (90.0%) in the tacrolimus ointment group and 31 patients (77.5%) in the corticosteroid regimen group. There were few discontinuations, but for those who did, the most common reason was lack of efficacy (tacrolimus ointment, n = 1, corticosteroid regimen, n = 4). The median number of days in the study was 363 in the tacrolimus ointment group, and 361 in the corticosteroid regimen group. The median numbers of treatment days were 255 and 327, respectively.
Table I. Patient baseline demographics and efficacy parameters at baseline, and months 6 and 12
| Tacrolimus 0.1% | Corticosteroid | |
| Age (years), mean ± SD | 29.2 ± 10.1 | 29.3 ± 10.7 |
| Sex, n (%) | ||
| Male | 9 (22.5) | 10 (25.0) |
| Female | 31 (77.5) | 30 (75.0) |
| Duration of AD (years), mean ± SD | 26.3 ± 10.2 | 27.4 ± 11.1 |
| Severity of AD, n (%) | ||
| Moderate | 18 (45.0) | 19 (47.5) |
| Severe | 22 (55.0) | 21 (52.5) |
| Affected BSA %, median (Q1–Q3) | ||
| Baseline | 58.3 (30.1–75.0) | 62.0 (28.1–83.5) |
| Month 6 | 5.4 (1.5–28.4)*# | 15.5 (5.6–48.8)* |
| Month 12 | 5.5 (1.9–42.3)* | 12.8 (3.1–42.3)* |
| EASI score, median (Q1–Q3) | ||
| Baseline | 21.3 (11.0–31.8) | 20.1 (12.7–37.9) |
| Month 6 | 3.2 (1.4–9.1)*# | 7.1 (3.0–17.9)* |
| Month 12 | 3.5 (1.7–12.0)* | 6.4 (2.4–15.4)* |
| Eczema score for head and neck, median (Q1–Q3) | ||
| Baseline | 18.0 (12.0–24.0) | 20.5 (12.0–32.0) |
| Month 6 | 4.0 (1.3–8.0)*## | 12.0 (4.0–20.0)* |
| Month 12 | 4.0 (2.0–11.3)*# | 9.5 (4.0–20.8)* |
| TEWL (g/m2h), median (Q1–Q3) | ||
| Head and neck | ||
| Baseline | 30.3 (20.6–41.7) | 35.2 (22.8–48.1) |
| Month 6 | 14.5 (11.4–20.1)*## | 20.7 (14.9–30.3)* |
| Month 12 | 14.5 (10.4–19.8)*# | 18.5 (11.8–28.0)* |
| Trunk and limbs | ||
| Baseline | 14.3 (9.5–19.4) | 16.2 (11.4–23.3) |
| Month 6 | 9.0 (7.9–11.4)* | 9.8 (7.0–13.3)* |
| Month 12 | 9.0 (6.7–11.7)* | 8.3 (6.7–12.8)* |
Intention-to-treat population. *p ≤ 0.001 vs. baseline, Wilcoxon test.
#p ≤ 0.05 vs. steroid, ##p ≤ 0.01 vs. steroid, Mann-Whitney test.
AD: atopic dermatitis; BSA: body surface area; EASI: Eczema Area and Severity Index; (Q1-Q3): interquartile range; TEWL: transepidermal water loss.
Clinical efficacy
The proportion of patients with ≥ 60% improvement in mEASI at month 3 was similar for both groups: 77.5% (n = 31) in the tacrolimus group and 72.5% (n = 29) in the steroid group. Affected BSA, EASI and mEASI scores improved in both treatment arms over 12 months of treatment. The improvement was significantly greater in the tacrolimus ointment group for each parameter at month 6 (Table I). This is consistent with the results from the large 6-month multi-centre study, in which the efficacy of tacrolimus ointment for these parameters was significantly greater than that of the corticosteroid regimen (p ≤ 0.01) (17). At month 12 the efficacy parameters for tacrolimus ointment were close to the month 6 results, with a median affected BSA improvement of 91%. The efficacy parameters for the corticosteroid regimen continued to improve slightly between months 6 and 12, with a final median affected BSA improvement of 79%. No significant difference in the efficacy parameters could be seen between the groups at month 12; this was probably due to the smaller difference in affected BSA between the groups at month 12, and the relatively small patient numbers.
At month 12, 57.5% (n = 23) of patients receiving tacrolimus were rated by their physician as having a response of “cleared or excellent” for the global evaluation of clinical response, compared with 42.5% (n = 17) receiving the corticosteroid regimen (p = 0.26). When the head and neck region was considered separately, 60.0% (n = 24) of the tacrolimus-, vs. 30.0% (n = 12) of the corticosteroid-treated patients were rated as “cleared or excellent” by the physician (p = 0.01). We also separately analysed the eczema score (area and individual signs) for the head and neck region, which represents 10% of the total EASI score. The scores were significantly lower in the tacrolimus group than in the steroid group at both month 6 (p ≤ 0.01) and month 12 (p ≤ 0.05).
Transepidermal water loss
TEWL decreased from baseline in both tacrolimus- and steroid-treated patients at month 12 for both the combined sites on head and neck, and trunk and limbs (p < 0.001). TEWL values for head and neck at month 12 were significantly lower in the tacrolimus group than in the steroid group (p = 0.04), which was in accordance with the lower eczema score for the head and neck in the tacrolimus group at month 12. TEWL for trunk and limbs did not differ between the treatment groups at month 12 (Table I).
Recall antigens
Both treatment groups experienced a significant increase in the Merieux score from baseline to month 12 (tacrolimus p = 0.001, steroid p = 0.04) (Fig. 1). No significant increase in the Merieux score could be seen in either group at month 6 (tacrolimus p = 0.21, steroid p = 0.19). The difference in the Merieux score between the groups was non-significant at month 12 (p = 0.4).
The number of positive antigen responses increased significantly in the tacrolimus ointment group after 12 months of treatment (p = 0.003). In the corticosteroid regimen group there was a numerical, but non-significant increase in the number of antigens (p = 0.09). The difference between the groups at month 12 was non-significant (p = 0.46).
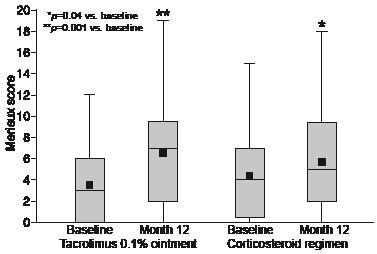
Fig. 1. Improvement of recall antigen reactions during treatment, as shown by the Merieux score. The results are presented as box-plots with the median value represented by a line across the box, and the mean by a smaller black box.
Serum total IgE
S-IgE levels at baseline differed between the two groups despite that other patient demographics, such as disease severity and EASI, were well balanced. Baseline median S-IgE was 659 kU/l in the tacrolimus group and 1523 kU/l in the corticosteroid group (p = 0.03). No significant decrease could be seen in either group at month 12. When all patients (tacrolimus ointment and corticosteroid treated) with at least 60% improvement in affected BSA at month 12 (n = 53) were analysed, median S-IgE decreased from 666 kU/l at baseline to 584 kU/l at month 12 (p = 0.02). In patients with at least 90% improvement in affected BSA at month 12 (n = 29) median S-IgE decreased from 532 kU/l at baseline to 383 kU/l at month 12 (p = 0.009). S-IgE for all patients (n = 80) correlated with affected BSA at baseline (r = 0.40, p < 0.001) and at month 12 (r = 0.49, p < 0.001). There was an inverse correlation between S-IgE and recall antigens (Merieux score) for all patients (n = 80) at both baseline (r = –0.40, p < 0.001), and month 12 (r = –0.34, p = 0.002).
Safety
Adverse events occurred in 40 patients (100%) in the tacrolimus ointment arm and 34 patients (85.0%) in the corticosteroid arm. The difference between the treatment arms was statistically significant (p = 0.03), and was accounted for mainly by the higher incidence of the well-known application-site skin burning sensation with tacrolimus ointment. The other common adverse events were flu syndrome and folliculitis. Flu syndrome was observed in 22 of the tacrolimus- and 16 of the steroid-treated patients during the study (p = 0.26), and folliculitis in 20 and 17 of the tacrolimus- and steroid-treated patients, respectively (p = 0.65). Infections (e.g. viral and bacterial skin infections, folliculitis, and flu syndrome), which in the opinion of the investigator probably or possibly could be related to treatment, occurred during the study in 26 patients (65.0%) receiving tacrolimus ointment and in 17 (42.5%) receiving the corticosteroid regimen (p = 0.07). Two patients in the steroid group showed signs of skin atrophy; one with striae of legs, observed during the last 3 months of treatment, and one with subcutaneous hematomas, which resolved when treatment was ended. No serious adverse events or deaths were reported during the study in either treatment arm.
DISCUSSION
This one-year, double-blind study showed that tacrolimus treatment was significantly more effective than a corticosteroid regimen at month 6. At month 12 tacrolimus treatment was numerically more effective, but the difference was non-significant, possibly due to the limited number of patients. Tacrolimus treatment was more effective than hydrocortisone acetate in the head and neck area at month 12, which was seen both for the head and neck eczema score and TEWL. Both treatments significantly decreased TEWL, probably by decreasing inflammation in the skin compartment. Active inflammation decreases filaggrin expression in the skin (20), which may lead to impaired barrier function (21). This allows environmental antigens and staphylococcal enterotoxins to penetrate the skin to further exacerbate the inflammation (22).
In this trial the use of study medication was not restricted, and showed the high number of treatment days required to manage moderate-to-severe AD effectively. In the corticosteroid group the number of treatment days was higher than might be considered safe, and signs of skin atrophy were seen in two patients. A previous 12-month study with a medium-potency corticosteroid, triamcinolone acetate, also reported skin atrophy and striae (15). Additional potentially harmful effects of corticosteroids include up-regulation of protease enzymes that could impair the skin barrier function (21). The main difference between topical corticosteroids and tacrolimus ointment is that long-term use of tacrolimus ointment does not decrease collagen synthesis, and thereby does not impair the structural integrity of the skin (23, 24). Tacrolimus ointment can be used over the longer term, or intermittently to control flares of AD. Two previous safety studies suggest that long-term intermittent use of topical tacrolimus in AD leads not only to improved clinical condition but also to a decrease in the use of tacrolimus ointment over a period of 12 months (10, 25).
The observed increase in the Merieux score after one year of topical tacrolimus or corticosteroid treatment reflects improvement in cell-mediated immunity as the signs and symptoms of AD improve. The current results are in direct contrast to those seen after systemic immunosuppressive treatment with cyclosporine, which is accompanied by a decrease in cell-mediated immunity (3). Tacrolimus and cyclosporine are both inhibitors of calcineurin, and the contrasting results on cellular immunity suggest that the effect of tacrolimus in AD is mainly in the skin.
Increased levels of IgE are common in AD, and reflect sensitization by environmental antigens and increased Th2 activity. Earlier studies have suggested a correlation between S-IgE levels and the degree of eczema (26). In this study we were able to confirm a correlation between S-IgE and BSA/EASI, and show an inverse correlation to recall antigens. Most importantly the results show that effective (at least 60% improvement) topical treatment of AD decreases S-IgE levels significantly. These results suggest that while a certain percentage improvement in affected BSA is reflected in a decrease of S-IgE level, the best results are obtained when the remaining affected BSA is as small as possible. The role of S-IgE in AD is not fully understood, but epidemiological data suggest a contributory role for immunological processes mediated by IgE in the onset and course of AD, especially in patients with severe disease (27).
In conclusion, long-term treatment with 0.1% tacrolimus ointment appears to be at least as effective as a corticosteroid regimen for the trunk and extremities, and more effective in the face and neck area. Both topical tacrolimus and corticosteroids increase skin recall activity, and decrease S-IgE in patients with good treatment response. These results suggest that skin inflammation in AD should be treated effectively, which could lead to an improvement in the Th1/Th2 balance in the skin, and to long-term improvement in the severity of the AD.
ACKNOWLEDGEMENTS
Dr Erik Mandelin is acknowledged for statistical advice. Tacrolimus ointment, Multitest devices, and patient visits for the study were supported by Astellas Pharma. J Mandelin has received research support from the Wilhelm och Else Stockmann Foundation, Finska Läkaresällskapet, and the Liv och Hälsa Society. Editorial support was provided by Dr Daniel Booth and funded by Astellas Pharma.
Conflict of interest: J. Mandelin, A. Remitz, H. Virtanen and S. Reitamo have spoken on behalf of Astellas Pharma at national and/or international meetings.
REFERENCES
